Autobullectomy: Disease Itself Relieved The Dyspnoea of Patient. Can It Happen?-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS INTERNATIONAL JOURNAL OF PULMONARY & RESPIRATORY SCIENCES
Abstract
The medical masters of yester years noted the great
importance of the actions of Nature in their writings. For instance,
Julius Cohnheim was emphatic that autopsies “are all in a manner
experiments instituted by nature, which we need only rightly interpret
to get a clear idea of the causes, laws of growth, and significance of
the tumour.” Indeed, as Nature has it, there is a “bare” area of the
liver. Moreover, this area is adjacent to the right adrenal gland.
Furthermore, as Bourne depicted, the position of the adrenal gland is
probably not fortuitous but related to some evolutionary factor.
Therefore, in line with my other practical papers, it is hypothesized
that, in cases of right lung cancer, a block containing hepatic and
adrenal deposits should be obtained. Then, special staining of the
individual lymphatic and blood vessels should be carried out. In all
probability, this process will reveal the routes of spread, especially
with reference to the interconnections of the individual metastases
present in both the liver and the adrenal gland. In other words, the
metastatic patterns will confirm or confute the concept of the
potentiality of hepatic metastasis in terms of being able to progress
further to the adrenal gland.
Bullous lung disease is a common presentation in
patients with chronic obstructive pulmonary diseases (COPD) and the
upshot of the inhalation of combusted tobacco products. Its occurrence
in female is very unusual. The development of small multiple bullae are
common, but the existence of giant bullae is usually erratic. The giant
pulmonary bulla occupies one third of the involved hemi-thorax and
characterized by the existence of centrilobular emphysema in the
non-bullous lung. Giant bulla slowly increases in size over time and
causes compressive atelectasis of lung parenchyma resulting respiratory
compromises [1]. Sometime air reabsorbs spontaneously leading to
shrinkage and regression of bullae known as autobullectomy [2]. Eleven
cases of complete resolution and six cases with partial regression of
giant bullae are recorded in the English literature [3]. Here, we are
discussing a case of spontaneous resolution of giant bullae following an
infectious episode in an older age female managed symptomatically.
A 50 years old female with a previous history of
twenty pack-years tobacco smoking came to the pulmonary outpatient
department with complaints of progressive increase in breathlessness on
exertion since one year and modified medical research council (MMRC)
grade 2 to grade 3 in last one month along with cough, mucoid
expectoration and fever of twenty days duration. She was neither
diabetic nor hypertensive. On admission, she was febrile, her pulse rate
was 110 beats/minutes, blood pressure 130/90 mm of Hg, respiratory rate
30breaths /minutes and oxygen saturation was 85% on room air.
Chest auscultation revealed decreased intensity of
breath sound in left intraclavicular, suprascapular, upper
interscapular and axillary area with rhonchi in other areas
on both sides. Her all routine blood investigations were
within normal limits including human immunodeficiency
virus (HIV) serology except polymorphonuclear (P>95%)
leukocytosis (total leukocytosis count 15000/mm3).
Sputum for acid fast bacilli (AFB) was negative and
pyogenic culture was sterile. Arterial blood gas (ABG) on
room air revealed PaO2-45 mm Hg, paCO2-40 mm Hg and
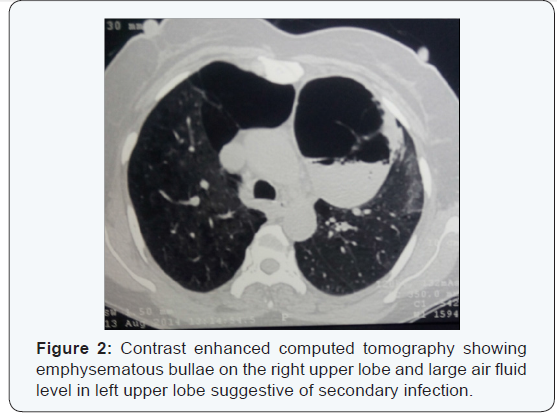
PH-7.35. Her chest x-ray showed an air fluid level on the
left upper zone with a few calcified parenchymal lesion
and hyper lucent area in the right upper zone (Figure 1).
With the provisional diagnosis of left side lung abscess
with chronic obstructive airway disease, she was started
oxygen inhalation by nasal prong at 2-4 litre per minute,
broad spectrum antibiotic, inhaled bronchodilators and
symptomatic treatment.
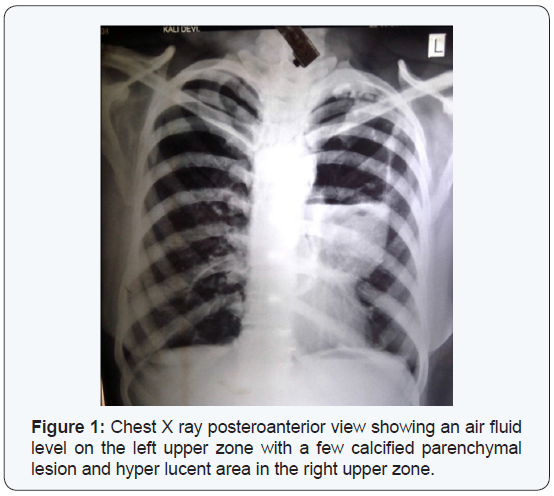
After 4-5 days, she didn’t show much relief in fever
and leukocytosis still persisted. Later, a contrast enhanced
chest tomography (CECT) scan revealed emphysematous
bullae on the right upper lobe and large air fluid level
in left upper lobe suggestive of secondary infection
(Figure 2). Fibre optic bronchoscopy was absolutely
normal, Bronchoalveolar lavage fluid taken from left
upper lobe was sent for AFB stain, gram stain, pyogenic
culture sensitivity (Pyogenic C/S), fungal culture and
mycobacterium tuberculosis culture by bactec method.
AFB stain was negative while the gram stain showed
gram negative bacilli and Pyogenic C/S naked klebsiella pneumoniae with negative other cultures.
Patient’s antibiotics modified according to culture
reports along with inhaled bronchodilator and
symptomatic treatment. After seven days, her leucocyte
count turned to normal. Patient became afebrile and
showed clinical improvement in severity of dyspnea and
cough. Repeat ABG revealed PaO2-85 mm Hg, paCO2-38
mm Hg and PH-7.38 on room air. She was discharged on
oral antibiotics for next 15 days with bronchodilators and
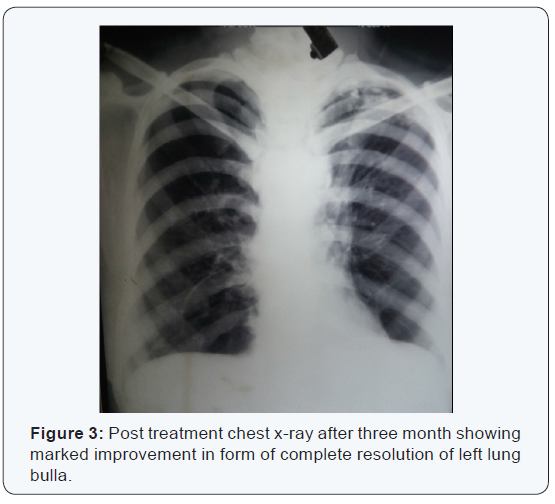
advised to quit smoking. Subsequent chest x-ray after
three month showed improvement in view of complete
resolution of left lung bulla (Figure 3)
Pulmonary bullae are pathological air space dilatations
> 2 cm in diameter, occurring distally at the terminal
bronchioles. Giant pulmonary bullous disease (vanishing lung syndrome) is characterized by the presence of giant
bullae in one or both upper lobes, conquering one-third
of the hemi thorax, asymmetrical and squashing nearby
normal lung parenchyma. It was first described by Bruke
in 1937 [4]. It has male predominance, occurs foremost
in smokers with doubtful cause. But in our case it was a
female with smoking history of twenty pack year. There
are two hypotheses which can explain its occurrence: -
protease-anti protease and oxidant-anti oxidant theory.
Firstly, it has been assumed that smoking enflame the
subcellular inflammatory mediators that letdowns
the balance in alveolar proteases and anti-proteases,
triggering a chain reaction at the cellular level that sooner
or later hints to destruction of alveolar walls. Secondly,
oxidative stress results from an imbalance between
oxidant and antioxidant proteins causing destruction of
lung parenchyma [5].
The gradual expansion of giant bullae is frequently
perceived, but the natural history is volatile and
pathophysiological mechanism of expansion is still
uncertain. Two theories explain its expansion; First the
elastic recoil theory by Morgan et al, bullae enlarge due
to comparatively grander elastic recoil of adjacent lung
parenchyma or in other words, adjoining lung tissue
retracts away from the pathologically dilated air space.
Second, the ball-valve theory, ball-valve affects proximal
airways causing dilation of the airspaces distal to the
terminal bronchioles. This check-valve phenomenon
increases positive end expiratory pressures within the
bullae endorsing a gradual expansion. Increase pressure in
the bulla cause compression of lung parenchyma, reduce
lung compliance and increase work of breathing; further
dead space fraction increases with bullae formation hence
gas exchange also hampered [6]. Atelectasis and even
mediastinal shift can also occur with giant bulla.
The clinical appearance vary from asymptomatic
bullous lung disease to mild cough, dyspnoea and fever to
severe lower respiratory infection and influenced by size
and infective pathology in bulla, adjacent lung parenchyma
and lung compliance that explain the need of mechanical
ventilator support [7]. The infected emphysematous
bulla (air fluid level) is more symptomatic and warrants
an aggressive management strategy. Bhardwaj et al. [8] explain the formation of air fluid level by two means.
Firstly, the reactive collection of air fluid level appears
due to peri-bullous pneumonitis and surrounding lung
parenchymal inflammation. Secondly, the loss of airway
communication between the bulla and larger airways
due to inflammatory mucus plugging causing inadequate
drainage of sterile fluid subsequent development of air
fluid level as seen in our case. The differential includes
lung abscess, pulmonary fungal infections such as
aspergillosis, pulmonary tuberculosis, cavitory lung
cancer - mostly squamous cell lung cancer and emphysema
with congestive heart failure.
Management is controversial and should be couturier
for each patient based on severity of presentation.
Persistent dyspnoea due to giant bulla and development
of secondary pneumothorax are most common indications
for bullectomy. An infected bulla in itself is not an indication
for bullectomy. The pathophysiologic mechanism of
spontaneous resolution or regression of giant bullae is
not well understood. Usually, spontaneous resolution
and regression of the bullae occurs due to an infectious
process. It is hypothesized that airway inflammation in
connotation with the infected bullae results in closure of
the communication between the airway and the bullae.
The gases within non-communicating space are now
slowly absorbed, resulting loss of volume and eventually
collapse of the giant bullae [9]. As this hypothesis explains
spontaneous resolution of bulla in our case. Sometimes,
tumour, mucous plug or a blood clot can also barricade
an already bargained bronchial communication ensuing
in a closed space [10]. Smoking cessation also improves the lung function as it decreases airway irritations. The
uses of inhaled bronchodilators and anti-inflammatory
medication also play a vital role in the resolution or
regression of the giant bullae as they decrease in airway
inflammation and thereby relieved a check-valve hence
improve in severity in dyspnoea as in our case [11].
Spontaneous resolution of giant bullae also known
as autobullectomy is an ignorant event and follows an
infectious event. The giant bulla closely mimics to lung
cancer and lung abscess so all patients should undergo
direct visualization of airway by fibre-optic bronchoscopy.
Smoking cessation and intensification of inhaled
bronchodilators should be instituted in all patients with
giant bullae that may mitigate its progression to ventilator
failure. The early suspicion and diagnosis by the treating
physician can avert the need for a surgical bullectomy in
these patients and decline the morbidity and mortality.
Our case is of interest not only because of the rarity with
which spontaneous regression has been reported in the
literature, but also because it was associated with such
dramatic improvements in severity of dyspnoea, partial
pressure of oxygen and arterial blood gas.
To know more about Open Access International
Journal of Pulmonary & Respiratory Sciences please click on: https://juniperpublishers.com/ijoprs/index.php

Comments
Post a Comment