Deadly High Altitude Pulmonary Disorders: Acute Mountain Sickness (AMS); High Altitude Pulmonary Edema (HAPE) and High Altitude Cerebral Edema (HACE): A Clinical Review-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS INTERNATIONAL JOURNAL OF PULMONARY & RESPIRATORY SCIENCES
Abstract
Mountain Sickness, also called High Altitude
Sickness, is specifically a triad of different disorders, in order of
increasing seriousness: Acute Mountain Sickness (AMS); High Altitude
Pulmonary Edema (HAPE) and High Altitude Cerebral Edema (HACE). These
three disorders, with relatively unimportant small variations seen in
some Pulmonology Textbooks, because these are so serious, they are all
potentially deadly pulmonary disorders and we will discuss these three
major, deadly disorders. Each one, starting with AMS, can progress
rapidly to HAPE and then HACE. The two authors of this article have over
half a century of high altitude mountaineering experience. They have
also had and still do have, for the last twenty years, an NGO,
Non-Profit Medical Organization (Wilderness Physicians
www.wildernessphysicians.org) that specifically deals with outdoor
medical issues, wilderness search and rescue, providing hospital level
care in the wilderness and also disaster medicine. Since spring is
rapidly approaching and many “weekend backpackers” will start going into
the mountains, we present this paper with the truths and fallacies of
this triad of disorders to refresh the memories of physicians who treat
these disorders, either in the field or in the hospital.
Abbreviations: AMS: Acute Mountain Sickness; HAPE: High Altitude Pulmonary Edema; HACE: High Altitude Cerebral Edema; DVT: Deep Vein Thrombosis; PE: Pulmonary Embolism
The mildest form of altitude sickness is Acute
Mountain Sickness (AMS). Where and how does acute mountain sickness
happen? Most people in “relatively” good physical condition, remain
feeling well up to altitudes of about 2500meters (8200 feet), the
equivalent barometric pressure to which most modern airplane cabins are
normally pressurized. However, even at around 1500meters (4920 feet)
above sea level, patients may notice more breathlessness than normal
during exercise and night vision may become impaired due to lack of
oxygen to the ocular apparatus. Above 2500meters (8200 feet), the
symptoms of altitude sickness usually become more noticeable.
Acute Mountain Sickness is sometimes colloquially
referred to as altitude sickness or mountain sickness; in South America
it is called Soroche, in China it is called Jíxìng Gāoyuán Bìng and in Nepal it is called Tīvra Pahāḍa Rōga.
The most prominent symptom of AMS is usually a severe
headache. Most people also experience nausea, vomiting, dehydration,
lethargy, dizziness and poor sleep patterns. Symptoms are very similar
to a severe, alcohol-induced hangover.
Anyone who travels to altitudes over 2,500meters
(8,200 ft.) is at risk for AMS. Normally it does not become noticeable
until the patient has been at that altitude for a few hours. Part of the
mystery of acute mountain sickness is that it is difficult to predict
who will be affected. There are many stories of fit and healthy people
being badly limited by symptoms of acute mountain sickness, while older
companions have felt fine.
There are a number of factors that are linked to a
higher risk of developing the condition. The higher altitude you achieve
and the faster your rate of ascent, the more likely you are to get
acute mountain sickness. If you have a previous history of suffering
from acute mountain sickness, then you are probably more
likely to get it again. Older people tend to get less AMS – but this
could be because they have more common sense and ascend
less quickly. Physical fitness is a suspected key factor, obviously
because the patient is in better condition. Smokers are at a
much higher risk of AMS due to already having decreased lung
function and lung elasticity, combining that with low oxygen
concentration at higher altitude increases the probability of
AMS, HAPE and HACE [1].
There is much less oxygen high in the mountains so it is
reasonable to accept the fact that travelling to high altitude will
cause people to feel sick. The problem is, how this shortage of
oxygen actually leads to altitude sickness is not fully understood.
Some scientists believe that it is due to swelling of the brain but
the evidence for this hypothesis is not conclusive. The theory
is that in susceptible individuals, swelling could cause a small
increase of the pressure inside the skull and lead to symptoms of acute mountain sickness. The swelling may be due to increased
blood flow to the brain or any increased permeability [2] of blood
vessels in the brain caused by a decrease in the pO2. Altitude
sickness has three forms. Mild altitude sickness is called acute
mountain sickness (AMS) and is quite similar to a hangover - it
causes headache, nausea and fatigue. This is very common: some
people are only slightly affected, others feel very sick. However,
if a patient has AMS, this should be taken as a warning sign that
this patient is at risk of developing the serious forms of altitude
sickness: HAPE and HACE. Both HAPE and HACE can develop
rapidly and be fatal within hours.
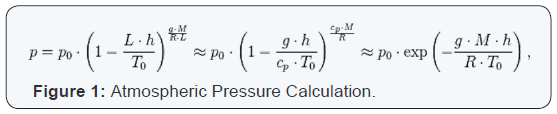
Atmospheric Pressure (also called Barometric Pressure) at
sea level is 14.7 psi (101.3 kPa). For calculating any atmospheric
pressure within the troposphere (from the surface of the earth
up to an altitude of about 12 miles or 20 km.) use this simple
formula [3] Figure 1.
Where the Constant Parameters are as Described Below
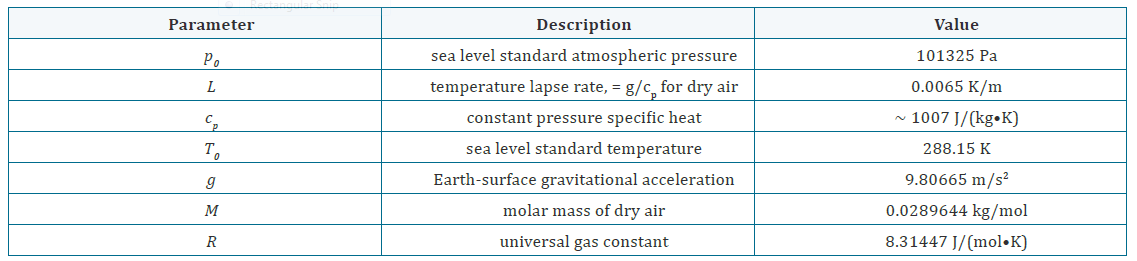
This ability to calculate the atmospheric pressure can quite
accurately help with treatment of the patient, however we will
repeat this several times, the single most important treatment is
to evacuate the patient down the mountain.
It is better to prevent acute mountain sickness than to try
and treat it! The patient needs to follow the “Golden Rule
of Mountaineering” and ascend slowly, which will give their
body time to acclimatize as they ascend. They will be less
likely to develop AMS. If a back packer has been climbing for
any amount of time, they will see the most experienced (and
smartest) mountaineers climbing at a SLOW, steady pace. This
is not because they are old and decrepit, this is because they are
smart and are slowly acclimatizing to the increase in altitude.
However, if a mountaineer needs to go up more quickly, they
could consider taking a drug called acetazolamide (also known
as Diamox). Acetazolamide is a carbonic anhydrase inhibitor
that is used for the medical treatment of glaucoma, epileptic
seizures, idiopathic intracranial hypertension, altitude sickness,
cystinuria (a rare condition in which stones made from an amino
acid called cysteine form in the kidney, ureter, and bladder),
periodic paralysis, central sleep apnea and dural ectasia (a
widening of the dural sac surrounding the spinal cord).There
is now good evidence that acetazolamide reduces symptoms of
AMS in trekkers and mountaineers, although it may have some
unusual side-effects such as causing the extremities to tingle or
food, especially fluids, taste strange.
As with any of the three forms of altitude sickness, if the
patient has acute mountain sickness, the best treatment is
descent. Painkillers may ease the headache, but they will not
treat the condition. Acetaminophen (Paracetamol) is the safest,
avoid these pain killers if they have codeine in them, as there are
no definitive studies on the effect of codeine on AMS. The patient
may be extremely thirsty, however increasing fluid intake should
be done with caution, as an increased intravascular volume can
exacerbate HAPE and HACE. If possible, a 22 Gauge (25 mm.)
I.V. Catheter (Venflon®) should be securely placed and either
flushed with heparin and capped off or if a long transport down
the mountain is expected in a Gamow Bag or on a stretcher, you can give 0.9% Normal Saline at a TKO (To Keep Open) rate or D5W,
also at a TKO rate. Avoid colloids because again, the effects of
colloids on the brain in HACE have not been extensively studied.
Acetazolamide may be helpful, especially if the patient needs to
stay at the same altitude. DO NOT however delay descending
with the patient in order to place an I.V. Catheter. The priority
is to get the patient to descend as rapidly as possible and the
patient should be strongly encouraged to descend, regardless
of the reason they need to stay up high, as they may rapidly
develop HAPE or HACE and die. Resting for a day or two at a
lower altitude might give their body time to acclimate and then
they can attempt to increase their altitude again, but even slower
than before. It is not clearly understood why, but once a patient
has had AMS, they are more susceptible to reoccurrences. It is
essential that the patient should NEVER go up higher, instead
of lower, if they have AMS as they will exacerbate the symptoms
and risk rapidly progressing to HAPE or HACE. This triad always
has to be thought of concomitantly during the treatment of
anyone with the initial symptoms of AMS.
- If you feel unwell, you have altitude sickness until proven otherwise
- Do not ascend further if you have any symptoms of altitude sickness
- If you are getting worse then descend immediately
- Do not descend alone, you don’t know what may happen
- Don’t die of altitude sickness.
Every year, people die of altitude sickness. All of these deaths
are preventable. If the person is travelling above 2500 meters
(8200 feet), this information could save their life.
Two things are certain to make altitude sickness very likely
- ascending faster than 500 meters = 1,965 feet) per day and
exercising vigorously (ie: backpacking). Physically fit individuals
are not protected – even Olympic athletes get altitude sickness.
Altitude sickness happens because there is less oxygen in the air
that you are breathing at high altitudes.
Gain altitude slowly, take it easy and give your body time
to get used to the altitude. The body has an amazing ability to
acclimatize to altitude, but it needs time. For instance, it takes
about a week to adapt to an altitude of 5000 meters (16,404 feet),
two weeks is better. When these two authors hiked up to “Base
Camp Everest South”(28°0′26″N 86°51′34″E) (5364 meters
= 17,598 feet) they took two weeks of slow backpacking from
Kathmandu to Base Camp Everest South. To save time and energy before beginning the trek to Everest Base Camp, it is possible to
take a plane to Lukla, but not recommended by these doctors due
to the sudden increase in altitude. Nevertheless, the two authors
of this article trekked from Kathmandu 1,400 meters (4,620
ft.) to Lukla at 2,843 meters (9,383 ft.) and rested overnight.
From Lukla, they trekked upwards to the City of Namche Bazaar,
which is often called the Sherpa Capital of Nepal because this
is where most Everest Expeditions hire their Sherpas and get
supplies. Namche Bazaar is situated at 3,440 meters (11,286 ft),
following the Valley of the Dudh Kosi River. It took about two
days of easy hiking to reach this village, which is a central hub
of the area and full of wonderful local people. Typically at this
point, climbers allow another day of rest for acclimatization,
which the two authors did. When the locals found out we were
doctors, they came to us with every ailment imaginable – but
it was a wonderful experience and these terribly poor people
paid us in some of the most wonderful food we have ever eaten
and their magnificent company. The children were an absolute
joy and they could not believe that a father and daughter doctor
team actually existed. I don’t think we cooked a single meal in
any of the towns we stopped in due to the wonderful generosity
of the Nepalese People. We then trekked another two days to Dingboche at 4,260 meters (13,976 ft.) before resting for
another day for further acclimatization. Another two days took
us to Everest Base CampSouth (5364 meters = 17,598 feet)
via Gorakshep, the flat field below Kala Patthar, 5,545 meters
(18,192 ft) and Mt. Pumori. The reason we relate our personal
trek into veryhigh altitudes is because neither one of us suffered
from any kind of AMS, one of us is past 40 and the other is in her
20’s! If you just fly in, you miss the beauty of the countryside, the
incredible people of Nepal, their hospitality and their incredible
love of life and nature and you are at a very high risk of AMS!!
HAPE stands for High Altitude Pulmonary Edema and this
termsimply means “excess fluid accumulation in the lungs”.
Everyone who travels to high altitude should know about this
triad (AMS, HAPE, HACE) and the fact that death can result
rapidly from these disorders, do not ignore the symptoms!
HAPE is a dangerous build-up of fluid in the lungs that
prevents the alveoli from opening up and filling with fresh air
with each breath. When this happens, the patient becomes
progressively more and more short of oxygen, which in turn
worsens the build-up of fluid in the lungs. In this way, HAPE can
be fatal within hours.
HAPE usually develops after 2 or 3 days at altitudes above
2500 meters (8,202 feet). Typically the sufferer will be more
breathless compared to those around them, especially on
exertion. Most patients will have symptoms of acute mountain sickness. Often, they will have a cough and this may produce a
white or pink frothy sputum. The breathlessness will progress
and soon they will be breathless even at rest. Heart rate may
exhibit tachypnea, the lips may be cyanotic and the body
temperature may be elevated. It is easy to confuse symptoms
of HAPE with a chest infection, but at altitude HAPE must
be suspected as your primary differential and the affected
individual must be evacuated to a lower altitude immediately,
preferably accompanied by the highest ranking medical person
by education(in order of preference: physician, nurse or
paramedic) on the mountain.
Unfortunately, it is currently impossible to predict who will
get HAPE. People who have had HAPE before are much more
likely to get it again. Therefore, there must be some factor that
puts certain individuals at high risk of the condition. However,
just like acute mountain sickness, there are some known risk
factors. A fast rate of ascent and the altitude attained will make
HAPE more likely. Vigorous exercise is also thought to make
HAPE more likely and anecdotal evidence suggests that people
with chest infections, symptoms of a common cold before ascent
or smokers [1] may be at higher risk. One very good axiom to
follow is to “climb high, sleep low” (Obrowski, M.H. – Denali –
1986 – unpublished). What this basically means that if you are
attempting to climb a high mountain in stages (such as Denali,
formerly known as Mt .McKinley – (5,190 meters or 20,310
feet), climb as high as you can on whatever number day you are
on, establish a camp and then go down AT LEAST 150 to 200
meters (492 to 656 feet) to sleep – you will sleep better and
exponentially reduce your chances of trying to sleep through a
miserable night. You will also feel much better in the morning.
In addition, while climbing, all experienced backpackers know
they should hike/climb for 45 minutes of every hour and take
a break for 15 minutes – giving the body a rest break helps with acclimatization. Whenever you take a break and feel
the slightest symptoms of AMS, HAPE or HACE, come down
immediately at least 150 meters (482 feet). As Mountaineering
Physicians who run a non-profit wilderness organization (www.
wildernessphysicians.org) for the past twenty years, we have
recovered many dead “macho men” off of a mountain or simply
had to leave them there as eternal popsicles to remind other
climbers of what not to do!! No organization, including ours, will
EVER risk the lives of their Rescue Physicians, Rescue Teamsor
Search and Rescue Dogs to drag a corpse off a mountain – this is
the brutal reality of High Altitude Mountaineering!!
Despite years of careful research the exact causes of HAPE
remain poorly understood. Fluid has been shown to fill up the
alveoli in the lungs preventing oxygen getting into the blood
and causing the vicious circle of events that can kill people with HAPE. As with many biological processes, many factors play
a role in this condition and there is good evidence to support
a number of theories about how this fluid accumulates in the
lungs.
Normally, oxygen gets into your blood and is supplied to the
body from your lungs. Each time you take a breath in, air rushes
into the tiny alveoli at the end of all the bronchioles in your
lungs. At the same time, blood from your heart is brought close
to these thin-walled alveoli so that oxygen can move into your
blood while waste products move out. Oxygen-rich blood then
returns to the heart and is distributed to the body. If, by accident,
a person inhaled a small object into their lungs, it would become
stuck in one of the airways branches. Little oxygen would get to
the downstream alveoli. To prevent this area of lung supplying
blood starved of oxygen back to the heart (and therefore the rest
of body), blood vessels in this area will constrict, self-protecting
the body.
At high altitudes however, this same process occurs and is a
cause of the disorder HAPE. The entire lung is starved of oxygen
and therefore the entire lung reacts in the same way – blood
vessels start constricting everywhere within the lung and not just
in small areas. The blood in these vessels is constricted and the
pressure goes up, the permeability of the vascular endothelium
increases and fluid is forced out of the blood and into the alveoli.
Reactive Oxygen Species (ROS) are formed in your blood when
a patient is starved of oxygen. Some of these highly damaging
molecules are produced as follows: The reduction of molecular
oxygen (O2) produces Superoxide (•O2−); Dismutation of
Superoxide produces Hydrogen Peroxide (H2O2); H2O2 in turn
may be partially reduced to a hydroxyl radical (•OH) or fully
reduced to water (H2O), which fills the alveoli. The hydroxyl
radical is so extremely reactive that it immediately removes
electrons from any molecule nearby, turning that molecule into
a free radical and so propagating a chain reaction.These highly
reactive molecules can directly damage the alveolar membranes
between the air and blood in the lungs, causing further fluid
leakage into the alveoli and worsening HAPE.
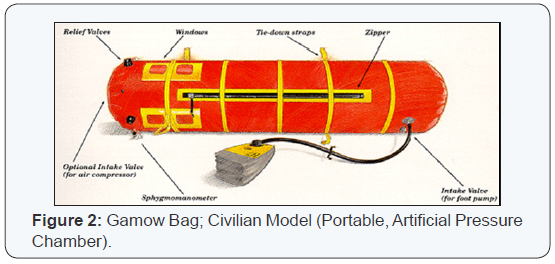
The most important treatment for HAPE is descent.
Providing extra oxygen and/or raising the air pressure around
a victim with a Gamow Bag (Figure 2) can partially reverse the
underlying process, lack of oxygen, but these measures are not a
permanent substitute for rapid descent down the mountain. The
patient is placed in a sleeping bag and then inside the Gamow
Bag. The foot pump is used to increase the internal pressure of
the bag and this in effect lowers the “altitude” that the patient
is experiencing. There is also a port that allows oxygen to
be connected and insufflated, helping increase the patient’s
pO2. Again, the patient still has to be rapidly moved down the
mountain as there is no way for a physician to physically touch the patient and treat him/her. The Gamow Bag is a temporary,
although extremely effective adjunct.
The primary author of this paper has personally seen the
Gamow Bag actually save the life of a patient on top of California’s
highest peak, Mount Whitney (14,505 ft. or 4,395 meters). This
author climbed Mt. Whitney with his Rottweiler in about 8 hours
and when he got to the top, there was a massive commotion going
on. A patient had literally dropped unconscious at the summit,
but unfortunately he was the group’s paramedic and was totally
unresponsive. The author took over and by the basic history he
could gather from the hysterical group, the patient had either
HAPE or HACE, although the author suspected HACE, due to the
rapid deterioration and unconsciousness. The author found that
they actually had a packaged, brand new Gamow Bag in their
medical supplies, but no one even knew what it was. We placed
the paramedic-victim in a sleeping bag, then into the Gamow
Bag; pressurized the Gamow Bagand hooked up the Rottweiler
by her harness to the bag. The dog dragged the patient all the way
down to a road that went about ⅓ of the way up the mountain,
for people that didn’t want to climb the mountain from the
base. (This was the problem, a relatively small climb on a high
mountain with absolutely no acclimatization). These people
had all their vehicles there but were from a different state, so we took one of the trucks with the patient, the author and the
Rottweiler in the back and we took the patient to the nearest
hospital, about a two hour drive at 100 mph (161 kph). In the
meantime, the author had opened the Gamow Bag, started an I.V.
TKO and eventually the patient made a full recovery. No drugs
were available as this was the paramedics’ personal medical kit
and paramedics in California are not allowed to possess or give
any drugs without a direct order from a physician. The Gamow
Bag saved his life for sure and is one of the best investments a
mountaineering group can make. Current 2016 pricing: $2,110;
€1,942; £1,465.
Some drugs can be helpful, but should only be used by
trained doctors, there for no dosing will be provided here as this
article can be read by anyone. Nifedipine is a drug that helps to
open up the blood vessels in the lungs. By doing so, it reduces
the high pressure in those vessels that is forcing fluid out into
the lungs. Following recent research, physicians may also give
the steroid, dexamethasone. Drug treatment should only ever be
used as a temporary measure; the best treatment is descent.
HAPE also causes breathlessness due the increased fluid
in the lungs. It is never normal to feel breathless when you are
resting - even on the summit of Everest. This should be taken
as a sign that the patient has HAPE and may die soon. HAPE
can also cause a fever and coughing up frothy, bloody sputum.
HAPE remains the major cause of death related to highaltitude
exposure with a high mortality in absence of adequate
emergency treatment.
Physiological and symptomatic changes often vary according
to the altitude involved. The Lake Louise Consensus Definition
for High Altitude Pulmonary Edema [4] has set widely-used
criteria for defining HAPE symptoms.
- The patient should have at least two symptoms [5]:
- Dyspnea at rest
- Cough
- Weakness or decreased exercise performance
- Chest Congestion
- The patient should have at least two signs [5]:
- Crackles or wheezing in at least one lung field
- Central Cyanosis
- Tachypnea
- d.Tachycardia
- Intermediate Altitudes (1,500 – 2,500 meters or 4,950 – 8,250 feet)
- Clinical symptoms are unlikely
- Blood oxygen levels remain >90%
- Clinical symptoms are common
- May develop after 2 to 3 days
- Blood oxygen levels may drop below 90% or lower during exercise
- Prior acclimatization will decrease the severity of the symptoms.
- Extreme Altitude (>5800 meters or 19140 feet)
- Blood oxygen levels are <90%, even at rest
- Progressive deterioration may occur despite acclimatization
If a travelling companion has symptoms of acute mountain
sickness and becomes confused or unsteady or develops an
extremely severe headache or vomiting, they may have the
life-threatening condition called High Altitude Cerebral Edema
(HACE).
There are many remedies touted as treatments or “cures”
for altitude sickness, but there is no evidence to support any of
them. The only chance the patient has is IMMEDIATE evacuation
to as low an altitude as possible. Put the patient in a Gamow Bag
if one is available.
HACE is high altitude cerebral edema and is a build-up
of fluid on the brain. HACE is extremely life-threatening and
requires urgent action.
HACE is the most severe form of acute mountain sickness
[6]. A severe headache, vomiting and lethargy will progress to
unsteadiness, confusion, drowsiness and ultimately a coma.
Drowsiness and loss of consciousness occur shortly before death.
HACE can kill in only a few hours, so the treating person must act
immediately. If you wait a “few hours” until it is light enough to
see, the patient will either die waiting to be evacuated or shortly
thereafter. A person with HACE will find it difficult to walk heelto-
toe in a straight line (ataxia) – this is a useful test to perform
on someone with severe symptoms of acute mountain sickness.
HACE should also be suspected if a companion starts to behave
irrationally or bizarrely. Protect the patient from hurting him
or herself by removing or hiding anything sharp or dangerous
objects (such as climbing axes) or weapons.
About 1% of people who ascend to over 3,000meters (9,900
ft.) get HACE. The lowest altitude at which a case of HACE has
been reported was 2,100meters (6,930 ft.). HACE can also occur
in people with HAPE and vice versa. Factors that increase the
risk of HACE are similar to those for acute mountain sickness and
HAPE. The faster the rate of ascent and the higher the altitude, the
more likely it is that HACE will develop. HACE is thought to occur
mainly in trekkers or climbers who have ignored symptoms of
acute mountain sickness and continued climbing higher rather
than staying at the same altitude or descending.
The cause of HACE, like HAPE, remains unknown. Several
factors may play a role including increased blood flow to the
brain. An increase in blood flow is a normal response to low
oxygen levels in the brain as the body needs to maintain a constant
supply of oxygen to the brain. However, if the blood vessels in the
brain are damaged, fluid may leak out of the vessels [7] and cause
HACE. The skull is an immobile encasement designed to protect
the brain, but any additional fluid will increase intracranial
pressure, contributing to HACE and in the extreme, causing an
Uncal Herniation (a subtype of transtentorial downward brain
herniation) and instant death.
As mentioned before, HAPE and HACE often occur together,
so as the treating physician, do not waste time trying to ascertain
which one the patient has, just get the patient evacuated to a
lower altitude as soon as possible.
Again, as with HAPE, rapid descent is the most effective
treatment of HACE and should not be delayed if HACE is suspected. A Gamow Bag (Portable Pressure Chamber - Figure
2), can be used as a temporary measure and, if available, oxygen
and a drug called dexamethasone should be given, but only by a
physician [8].
Altitude sickness occurs when an individual who is
accustomed to low altitudes rapidly climbs to a high altitude [8].
Altitude sickness is a potentially lethal complication of climbing
to altitudes above 8,000 feet (2,425 meters) [9-11]. Three
main syndromes of altitude illness may affect travelers: Acute
Mountain Sickness (AMS), High Altitude Pulmonary Edema
(HAPE) and High Altitude Cerebral Edema (HACE). The risk of
dying from altitude related illnesses is low, at least for tourists.
For trekkers to Nepal the death rate from all causes was 0.014%
and from altitude illness 0.0036%, soldiers posted to altitude
had an altitude related death rate of 0.16%.
Treatment of altitude related illness is to stop further
ascent and if symptoms are severe or getting worse, to descend
immediately! DO NOT DELAY!! Oxygen, drugs, Gamow Bags
and other treatments for altitude illness should be viewed as
adjuncts to aid descent, NOT AS PRIMARY TREATMENTS!
The Death Zone is the name used by mountain climbers for
high altitude where there is not enough oxygen for humans to
breathe. This is usually above 8,000 meters (26,400 feet). Most
of the 200+ climbers who have died on Mount Everest have died
in the death zone.
No human patients were used in the development and writeup
of this paper.
To know more about Open Access International
Journal of Pulmonary & Respiratory Sciences please click on: https://juniperpublishers.com/ijoprs/index.php

Comments
Post a Comment