Implications of Non-invasive Mechanical Ventilation in Lung Transplantation. Old and New Frontiers?-Juniper publishers
JUNIPER PUBLISHERS-OPEN
ACCESS INTERNATIONAL JOURNAL OF PULMONARY & RESPIRATORY SCIENCES
Abstract
As
lung transplantation has become more successful, the selection criteria
have broadened; however, some relative contraindications to lung
transplantation are controversial. Some programs consider mechanical
ventilation to be a major contraindication to lung transplantation
because airway colonization with bacteria may lead to nosocomial
infection and respiratory muscle deconditioning may necessitate
prolonged postoperative ventilatory support. Non-invasive mechanical
ventilation is accepted as a bridge to lung transplantation, but there
is little evidence to support its use outside this setting. Use of
non-invasive positive pressure ventilation (NPPV) has been reported as a
means of avoiding orotracheal intubation in cases of respiratory
failure, and in cases of refractory hypoxia; and several longitudinal
randomised studies have shown its superiority over conventional
ventilation.
In
1909, Meltzer and Auer published a study on continuous breathing
without respiratory movements obtained by introducing a continuous
stream of air and anaesthetic vapour into the trachea [1]. This can be
seen as the origin of mechanical ventilation, as it preceded the
subsequent development of methods for applying intermittent positive
pressure and orotracheal tubes with pilot balloon. In the last 30-40
years, important progress has been made due to better understanding of
the Pathophysiology of breathing, the emergence of new specialists in
intensive respiratory care, and technological development. Several
alternatives breathing support strategies have been designed that have
reduced the associated complications.
The
study adopted a case study research design. Theresearcher applied
survey approach with purposive samplingto select 27 respondents from
police investigators involvedin the investigations [36]. The conducted
extensive review ofliterature and obtained various preliminary factors
to be tested[37]. Hypothesis formulated to be tested for each factor
was:Null Hypothesis, H0: The identified factors have no
significantinfluence on effectiveness of murder procedures at
profiling;Alternative Hypothesis, H1: The identified factors
havesignificant influence on effectiveness of murder procedures
atprofiling; the researcher used questionnaires and interviewguides to
help in data collection. The questionnaires closed endedquestions with
Likert rating of 1-5 in addition to structuredopen-ended questions at
the end. Necessary permissions weresought from the National Commission
of Science, Technologyand Innovation and from county and police
authorities as wellas the respondents. Ethical guidelines for social
research wereadhered to during the process [38]. The researcher
interviewed some directors of the company to gain insights into the
problem.Sensitivity of the issue was a major limitation in the research.
Face
and content validity of the research instruments wasachieved when they
were subjected to review by an authoritywith good professional and
research standing and found to bevalid. The instruments were then tested
and adjustments madeaccording to recommendations given by experts whose
opinionwas sought by the researcher. Secondary data collection
frompublications, books, news reports, police preliminary reportswas
done. Secondary data from county criminal investigations office (CCIO)
in the county (Murang’a County) where the KihiuMwiri Company was located
proved useful in giving insights intothe study. Media reports also gave
highlights into the problemand led the researcher to follow up and
obtain even case numbersto verify the prosecution process and identify
gaps. Quantitativedata was analysed using descriptive statistics where
mean,mode and standard deviation were obtained [39]. One samplet-test
was performed and significance levels of the results noted.Correlation
analysis of variables was carried out to give insightinto how the
factors relate to effectiveness of murder profiling.
Mechanical
ventilation is an intervention that enables adequate gas exchange
during certain acute events. It is indicated in the following
circumstances:
- Insufficient alveolar ventilation, with elevated PCO2.Rapid elevation of PCO2 is accompanied by significantrespiratory acidosis; a more gradual increase can becompensated and better tolerated. There is no clear cut-offpH value beyond which a patient requires ventilation. Zwillchsuggested 7.30 [2], below which morbidity and mortality aresignificant.
- Diminished or unstable ventilation: manifests as aslower respiratory rate or even apnoea. It occurs in situationssuch as head trauma, drug overdoses or cerebrovascularaccidents. There is a risk of apnoea, so ventilation is indicatedeven when there is no hypercapnia.
- Severe hypoxaemia, which does not resolve with theadministration of oxygen through a mask
- Insufficient pulmonary expansion: can cause atelectasisand pneumonia. It can occur during general anaesthesia,trauma or acute restrictive pulmonary disease.
- Insufficient respiratory muscle function: such as inGuillen-Barré syndrome.
- Excessive respiratory effort: which the patient cannotmaintain. During an acute disorder, it usually starts withtachypnoea.
Complications can be due to the underlying condition,its severity, the intensive care setting and mechanicalventilation itself.
- Altered ventilation-perfusion ratio: perfusion increasesin dependent lung regions, while ventilation increases in therest.
- Reduced alveolar perfusion: high-pressure valuesin the airways, especially with hypovolaemia, can causecompression in the pulmonary capillaries, transformingfunctioning alveolar-capillary units into physiological deadspaces.
- Altered circulation: as intra-thoracic pressure increases,venous return diminishes, which in turn diminishes cardiacoutput and renal perfusion. This is further aggravated in thecase of hypovolaemia.
- Liver and kidney dysfunction: the use of PEEP has beenassociated with reduced portal and renal flow rates, whichcan cause dysfunction in these organs.
- Increased intracranial pressure: an increase in intrathoracicpressure causes reduced venous drainage from thehead.n
- Gastric distension: due to swallowing air becauseof leaks around the balloon in patients with orotrachealintubation.
- Altered acid-base balance: usually due to sub-optimalventilator adjustment.
- Air entrapment, dynamic hyperinflation and auto-PEEP: when the expiratory flow is blocked, exhalationmay not have completed before the next inhalation starts.Pulmonary volume and alveolar pressure, therefore, arestill high at the end of the exhalation, resulting in the samephysiological effects as excessive PEEP.
- Barotrauma: manifest as pneumothorax,pneumomediastinum or subcutaneous emphysema. Thecause is usually interstitial alveolar rupture, with subsequentdissection to the mediastinum or elsewhere.
- Volutrauma (ventilator-induced lung damage): theprecise mechanism is not clear, but it is associated withalveolar over distension.
- Nosocomial pneumonia: from oropharyngeal germs.
- Air way lesions: lesions caused during orotrachealintubation, tracheal stenosis, bronchoaspiration, andtracheal-oesophageal fistula.
- Muscle weakness: due to long-term use of musclerelaxants.
- Reduced oxygenation in ventilated patient: thereare several causes, such as ventilator or circuit problems,unfavourable evolution of the patient’s primary process, theonset of a new medical problem, or certain manoeuvres andinterventions.
The
use of continuous positive airway pressure (CPAP) inthe airways was
first suggested in 1981 to treat obstructivesleep apnoea [3]. The
application of CPAP through a mask forthis purpose was the first step in
the development of NPPV forpatients with chronic respiratory failure.
Generally speaking,there are two NPPV techniques: positive pressure
appliedcontinuously to the airway throughout the respiratory
cycle(CPAP); or positive pressure applied intermittently. In
CPAP,breathing is spontaneous and generated solely by the
respiratorymuscles. Intermittent positive pressure systems, meanwhile,
areapplied in one of two ways:
- pressure support ventilation, in which a certainpressure is applied to the airway during inhalation toimprove spontaneous breathing. The respiratory rate isdetermined by the patient and the tidal volume by theamount of inspiratory support pressure and factors such asinspiratory and respiratory effort. It is activated either whensystem pressure decreases or flow increases;
- bi-level positive airway pressure, which is similar toCPAP, but with pressure support. Inspiratory and expiratorypressure can be adjusted and the ventilator switches frominhalation to exhalation when flow changes are detected.
The
difference between inspiratory and expiratory pressureis the
non-invasive pressure support. Positive pressure can beapplied at the
end of exhalation (PEEP) with either of these twomethods. The success of
NPPV largely depends on the patient’sability to cooperate and
synchronise his or her breathing with theventilator because, unlike
invasive ventilation, the patient doesnot receive muscle relaxants. This
type of ventilation was initiallyused in patients with neuromuscular
disorders and chest walldiseases, subsequently extending its use to
other disorders [4].The use of NPPV was first described in 1989 to
circumvent theneed to intubate patients with acute respiratory failure
[5] and itwas subsequently described in COPD exacerbations [6]
reducingventilation time and duration of ICU admission, suggesting
thatNPPV could reduce ventilator-induced morbidity and the cost ofCOPD
exacerbations. Subsequent studies of patients with COPDexacerbations
[7,8] support the use of NPPV to circumventorotracheal intubation.
Use
of NPPV has also been described in acute respiratoryfailure due to
causes other than COPD: in patients with acutedecline due to restrictive
thoracic diseases [9] hypoxemicrespiratory failure without hypercapnia
(pneumonia, ADRS,cardiogenic oedema) [10] acute respiratory failure in
theimmediate post-operative period following extubation [11]; inpatients
who require orotracheal intubation and mechanicalventilation, NPPV can
be used in the “weaning” process [12]and also in patients with
respiratory failure who are notsuitable for orotracheal intubation [13].
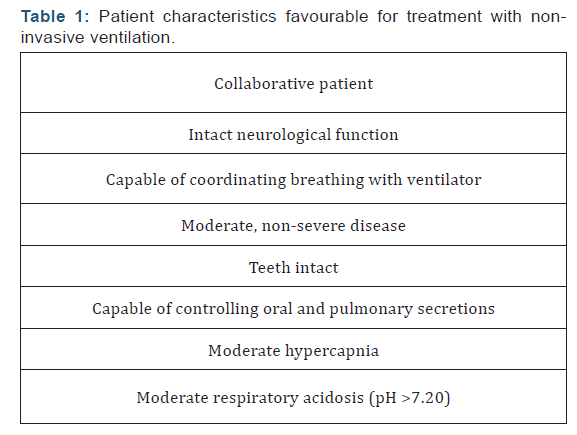
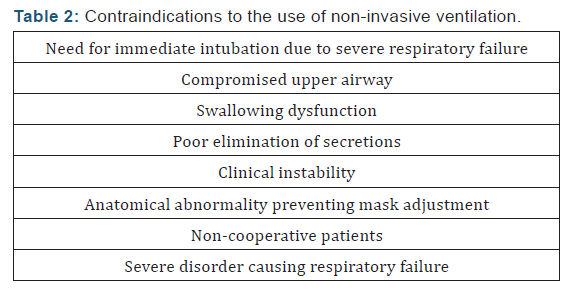
Appropriate patientscreening is crucial to ensure the success of NPPV
(Table 1) andto prevent use when contraindicated (Table 2). Unlike
invasiveventilation, non-invasive techniques do not require an
artificialairway (endotracheal tube or tracheostomy). A good interface
isessential. Both nasal and oronasal and facial masks can be used.Nasal
masks leave the mouth uncovered, enabling the patient totalk and eat,
but air loss through the mouth is common. Whatevertype is chosen, it
should always be a good fit.
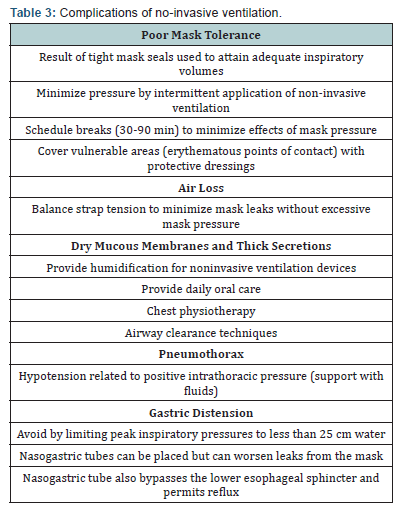
To
facilitate tolerance, it is good idea to initially use lowpressure.
Initial pressure support could be 4-10 cm H2O, PEEP:2-4 cm H2O,
inspiratory pressure: 8-12 cm H2O and expiratorypressure: 2-4 cm H2O.
The initial tidal volume ranges from 10 to15 ml/kg. As patient tolerance
increases, inspiratory pressureor tidal volume can be gradually
increased to enable smallreductions in PCO2 (5-10 mmHg). If oxygenation
is still low,expiratory pressure can be increased. Patients who respond
wellto the system will present lower respiratory rate, heart rate
andPCO2 after a few hours. The possible complications are shownin Table
3. Several studies have shown the efficacy of NPPVfor preventing
nosocomial pneumonia and other orotrachealintubation complications
[14-16]. As these patients are notsedated, complications due to
immobilisation are prevented andadequate nutrition is ensured. ICU stays
can be prevented. Itdoes, however, have some disadvantages: no airway
protectionand no direct access to the trachea for aspiration.
The
first references to lung transplantation date from the1940s and 1950s,
when authors such as Vladimir Demikhov andDominique Metras demonstrated
the viability of the surgicaltechnique in experimental animals [17].
Subsequently, in1963, James Hardy performed the first single lung
transplantin humans. The patient was a death row inmate who had
beendiagnosed with squamous cell carcinoma in the left lung
andemphysema. He only survived for 18 days, and died from kidneyfailure
[18]. Further attempts were made in the following years,but they
systematically failed due to infections, graft rejectionand problems
related to bronchial anastomosis healing. Itwas not until the 1980s when
the Toronto group, under theleadership of Joel Cooper, performed the
first successful single(1983) and double (1986) lung transplants, thus
establishingthe procedure as treatment for end-stage lung diseases
[19].Since then there has been significant progress in both
surgicaltechnique and overall patient management, and the procedurecan
now be safely performed with greater short- and mediumtermsurvival
rates. It is currently a valid therapy for some endstagelung diseases
with less than 2 years of life expectancy forwhich there are no further
medical options.
The diseases that most often
require this procedure are:emphysema-like COPD with or without
alpha-1-antitripsin deficit,interstitial diseases such as idiopathic
pulmonary fibrosis, septicconditions such as cystic fibrosis or
bronchiectasis, and primarypulmonary hypertension. The current trend is
to perform doublelung transplantation, especially in young patients, as
they providebetter quality of life and long-term survival, despite
greater perioperativemorbidity/mortality [20]. During surgery, the
airwayis routinely intubated with a left-sided double lumen tube
thatenables independent ventilation of both lungs. Immediatelyafter
surgery, patients are ventilated with a standard technique.FiO2 is
necessary to maintain the PO2 at over 70 mmHg. The tidalvolume is 12-15
ml/kg and PEEP is 5-7.5 cm H2O. The patient isextubated when there is
adequate gas exchange and mechanicalrespiration, usually after 24-48
hours. PEEP is not needed inCOPD patients who receive a single lung, and
a lower tidalvolume is used. This reduces hyperinflation of the native
lungand minimises compression of the transplanted organ.
Air entrapment by the native lung can cause other problems,such as high
airway pressure, CO2 retention and hypotensiondue to reduced venous
return. Volume reduction in the nativelung is required in extreme cases
to relieve compression in thetransplanted organ. Mechanical ventilation
is maintained forlonger, at least 48-72 hours, in patients with vascular
pulmonarydiseases who have received a single organ transplant,
duringwhich time they are sedated and receive muscle relaxants,remaining
in a position in which the native lung is lower,thus maintaining
inflation and drainage of the grafted organ.Standard tidal volume is
used but PEEP increases to 7.5-10 cmH2O. Mechanical ventilation is
prolonged in case of primary graftdysfunction, rejection or infection.
In these cases a tracheotomyshould be performed as soon as possible,
making the patientmore comfortable, increasing his or her mobility, and
enablingoral nutrition.
As
with any other type of surgery, respiratory complicationscan arise in
the post-operative period, such as atelectasis,pneumonia, pulmonary
oedema and acute respiratory failuredue to different causes, including
pulmonary thromboembolism.Post-operative respiratory failure can be
defined as the need tomaintain mechanical ventilation for longer than
usual for thesurgery in question, or the need to re-intubate an
extubatedpatient [21]. In lung transplantation other specific
problemscan also arise, such as vascular or airways
complications(stenosis, dehiscence), primary graft dysfunction,
pneumoniaand rejection. Nevertheless, acute respiratory failure is the
maincause of post-transplant mortality [22]. Special mention shouldbe
made of airway anastomoses, specifically dehiscence. In thesecases,
either invasive or non-invasive positive pressure canhinder management.
In severe cases in which a patient cannot beventilated because all or
most of the tidal volume is lost throughdehiscence, the only solution is
differential ventilation througha double lumen tube: optimal
ventilation in the dehiscence-freelung and ventilation with the lowest
possible pressure in theother lung.
Disorders
where NPPV can be used have already beenmentioned above. NPPV has been
described in general surgeryfor preventing acute post-operative
respiratory failure(prophylactic use) or for treatment of this condition
when itpresents [23,24], and it can be used both with continuous
(CPAP)and intermittent positive pressure. The expected benefits
are:increased lung gas volume, improved gas exchange,
reducedatelectasis, reduced respiratory effort, and circumvention
ofinvasive ventilation. In the case of lung transplantation, use ofNPPV
to avoid orotracheal intubation in cases of respiratoryfailure has been
reported. A study published in 2000 [14]randomised 40 solid organ
recipients (lung, liver or kidney) withacute hypoxemic respiratory
failure to be treated with NPPVor conventional therapy. There was a
sustained, statisticallysignificant improvement in oxygenation in the
NPPV group,with less need for invasive ventilation. The incidence of
sepsiswas also lower, as was ICU mortality rate, although there wasno
difference in hospital mortality rate. Another observationalstudy
conducted in 2001 [25], in which 21 patients undergoingbilateral lung
transplant presented acute respiratory failureafter extubation, found
that NPPV circumvented the need forendotracheal intubation in 85% of all
cases. Rocco, et al. [25]described a series of 21 patients (18 with
cystic fibrosis) who,after undergoing double lung transplant developed
respiratoryinsufficiency requiring ventilation support.
After being treated with NPPV through a facemask,orotracheal intubation
was avoided in 18 patients, who weredischarged from the ICU. Of the 3
who required intubation, 1survived and the other 2 died from septic
shock. It has beensuggested that NPPV can reduce extra vascular
pulmonaryfluid and restore pulmonary volume, reducing dyspnoea
andrespiratory effort. In 2009, Feltraco, [26] reported the use ofNPPV
for the treatment of refractory hypoxia due to primarygraft dysfunction,
describing two cases. In general, respiratorysupport is well tolerated
and resolves atelectasis and infiltrates,thereby avoiding orotracheal
intubation. The use of NPPVassociated with changes from a prone to
supine position, oreven combined with Trendelenburg, improves the
ventilationperfusionratio, suggesting that it could also be used for
otherlung conditions, which involve areas of dorsal-basal
non-recruitable atelectasis.
High
frequency percussive ventilation is a method that canbe applied by
intubation or a facemask [27]. It is a time-cycled,limited pressure mode
of ventilation. Cycles are delivered athigh frequency (200-900 cycles
per minute) in stages. This giveslow volume, high rate ventilation that
produces a more uniformgas exchange and better distal ventilation, while
facilitatingelimination of secretions. High frequencies (300-600
cyclesper minute) facilitate oxygenation, while low frequencies
(180-240) facilitate CO2 elimination. Feltraco [28] described itsuse,
combined with postural changes, in three patients whopresented
respiratory failure after extubation following doublelung
transplantation, thereby avoiding re-intubation in all three.Phrenic
nerve injuries during lung transplantation can be due todirect damage
caused during mediastinal dissection or distensionwhile manipulating the
pericardium and hypothermia. Aftersurgery, they can give rise to
complications such as atelectasis,pneumonia, hypoxaemia and
hypoventilation, increasingduration of mechanical ventilation and ICU
admission. NPPVhas been reported to reduce this time, and can even be
appliedoutside the ICU [29].
NPPV has also been
used during the pre-transplant period.Ventilator dependence has
traditionally been considered arelative contraindication for
transplantation, as the procedure isassociated with a higher mortality
rate in such patients [30,31].The presence of microbial colonisation of
the airway increasesthe risk of post-operative pneumonia. Prolonged
immobility canalso reduce a patient’s physical strength, increasing the
risk ofpost-operative complications. However, up to 3% of
transplantshave been performed in the US on ventilator-dependent
patients[32]. Ideally, in the case of invasive ventilation, the aim
shouldbe to extubate once the patient has overcome exacerbation
andperform the transplant when he or she is no longer
ventilatordependent.Only in carefully selected cases can
transplantationbe considered in patients who present progressive,
irreversiblerespiratory failure as the result of the evolution of their
condition.
The possibility of transplanting a
ventilator-dependentpatient is considered when respiratory failure is
the resultof the irreversible evolution of the underlying condition,and
other causes (such as respiratory infection, pulmonarythromboembolism,
heart failure, etc.) have been ruled out,providing the surgery can be
performed before the onset ofthe aforementioned complications derived
from mechanicalventilation, basically pneumonia and decline in physical
status.Pulmonary conditions are the main cause of morbidity-mortalityin
cystic fibrosis, and the use of NPPV has been reported toprolong the
life of end-stage patients until a donor appears,avoiding the
complications of invasive ventilation. Efrati, et al.[33] described a
series of 9 patients: four successfully underwenttransplant and 3 died
on the waiting list. The other two were stillalive when the paper was
published. Significant increase in bodymass index, improvement in pH and
PCO2, and better sleepsquality and everyday activities, with no
ventilation-relatedcomplications, have been reported. Further studies
describe thesuccessful use of NPPV while waiting for lung transplant
[34-37]particularly in cystic fibrosis patients.
In
the last 30-40 years, important progress in respiratorysupport has been
made due to better understanding of thephysiology of breathing, the
emergence of new specialists inintensive respiratory care, and
technological development.Several alternative respiratory support
methods have reduced thecomplications associated with invasive
mechanical ventilation.The diseases that most frequently require lung
transplantationare: emphysema-like COPD with or without alpha -1-
antitrypsindeficit, interstitial diseases such as idiopathic
pulmonaryfibrosis, septic diseases such as cystic fibrosis or
bronchiectasisand primary pulmonary hypertension. The current trend is
toperform double lung transplants, especially in young patients, asthey
provide better quality of life and long-term survival, despitegreater
peri-operative morbidity/mortality. In the case of lungtransplantation,
use of NPPV has been reported as a means ofavoiding orotracheal
intubation in cases of respiratory failure,and in cases of refractory
hypoxia; and several longitudinal,randomised studies have shown its
superiority over conventionalventilation.
To know more about Open Access International
Journal of Pulmonary & Respiratory Sciences please click on: https://juniperpublishers.com/ijoprs/index.php

Comments
Post a Comment