Six Minute Walk Test as a Criteria for Evaluation of Functional Status and Disability by One Time Single Measurement of Distance Walked in Six Minutes for Breathless Patients-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS INTERNATIONAL JOURNAL OF PULMONARY & RESPIRATORY SCIENCES
Abstract
6 Minute Walk Test is increasingly used in clinical
practice, as an objective measurement of functional status in patients
with moderate to severe impairment. It is one of the simple tests of low
complexity that measures the distance a patient can walk in 6 minutes.
The 6MWT is useful to assess response to medical interventions,
prognosis and as single measurement of functional status in cardio
respiratory disability.
Objective: There are few studies
done in India that prompted us to do this study with the objective to
evaluate functional status and disability by one-time measurement of
6-minute walk distance in patients with complains of breathlessness.
Methods: 121 Patients with complains
of breathlessness were registered for the study between June 2010 to
July 2011. Test procedures, purpose of the study were explained to
participants. The materials used, patient’s preparation and layout was
done using ATS-2002 guidelines. The participants were asked to walk at
their self-selected pace, attempting to cover as much distance as
possible in 6 minutes. The total distance walked in 6 minutes was
recorded.
Result: 121 patients were evaluated.
Mean age, height and weight was 56.75 years, 161.80cm and 64.93 kg
respectively. 101 patients completed the test, mean 6MWD was 390.08
meters (males 410.45, females 356.13m). 6MWD was significantly decreased
in cardio-pulmonary diseases.
Conclusion: In our study we
demonstrated that 6MWT can be safely performed even in patients with
advanced cardiopulmonary conditions. It is a useful marker for the
severity, progression and prognosis.
Walk testing was first advocated by “Balke” in 1963
to assess physical fitness. K. H. Cooper used 12MWT in healthy air force
personnel to demonstrate a strong correlation between maximal oxygen
consumption and maximal exercise testing. McGavin used walk test to
assess disability in COPD patients. 6MWT was introduced as functional
exercise test by Lipkin in 1986 which correlated with those of 12MWT and
cycle ergometry or treadmill. Although PFT continues to play a major
role in management and research (FEV1and FVC is used to assess severity
of breathlessness). The effectiveness and reliability
of the 6MWT became the most widely accepted protocol to assess
functional dusability. Walking is a measure of functional status of
daily activities. 6MWT is practical, simple, requires the ability to
walk. The distance a patient walks on a flat surface in 6 minutes is
used as a one-time measurement of functional status, or improvement
during rehabilitation. The test is self-paced, reflects the exercise
level needed for daily tasks [1], can be done by a technician. In 2002
ATS [1] outlined guidelines for 6MWT which reviewed the physiological
response to exercise. Guidelines were used to limit controllable factors
for variability (use of practice test, oxygen and medications prior to
or duringtesting).Technician does not walk with the patient to avoid
influencing the patient’s pace. Measurement of SPO2 is optional,
the test is usually terminated if the SP02 falls below 85% [2],
however it can be continued depending on experience of the
physician. In patients on long term oxygen therapy the 6MWT
can be performed with portable oxygen. The 6MWT should
be performed by a technician certified in cardio-pulmonary
resuscitation at the basic life support level although advanced
cardiac life support certification is desirable. Test is terminated
when there are signs of severe distress, confusion, dizziness,
diaphoresis, severe dyspnoea, fatigue. The patients were allowed
to stop if mild distress occurred, however they were asked to
resume walking. The patients were observed for 10-15 minutes
after the test, patients who started to walk but did not complete
the test were included in the study.
- Response to medical interventions in patients with moderate to severe cardio-pulmonary diseases.
- One-time measurement of functional status as a criterion for pulmonary affection and disability.
- Pre and post pulmonary surgery evaluation.
- Cardio pulmonary predictors of morbidity and mortality.
Inclusion Criteria
Stable patient’s between13-85 years of age with complaints
of breathlessness.
Exclusion Criteria
Myocardial Infarction in the preceding month, unstable
angina, resting heart rate>120/min, systolic BP >180 mm
Hg, diastolic BP >100 mm Hg, syncope, arthritis, skeletal or
neuromuscular diseases. Stable angina is not an absolute
contraindication (after taking anti angina drugs).
Test Procedure
The test was performed on a flat surface corridor of 15-meter
length (recommendation is 15-30 meters) marked with small
cones at the starting and end points and at every 3m distance,
the time and laps were recorded on a worksheet. Patients were
asked to wear comfortable clothes, take light meals, to sit for
10 minutes at the starting point for check on contraindication,
informed written consent was taken and details of test procedure
and risk associated were explained. Medical history with clinical
examination was undertaken along with BMI, BP, Borg scores for
dyspnoea and fatigue with resting heart, respiratory rate and
SPO2 were recorded after 10 minute’s rest, and after completion
of the test. Spirometry was performed and data collected as
per ATS guidelines. The patients were asked to walk while
attempting to cover as much distance as possible in 6 minutes.
Measurement
The total distance walked in meters in 6 minutes with
number of rest and stops during the test were also recorded.
Statistical Analysis
Statistical analysis was performed with statistical software
SPSS (Statistical Package for Social Sciences). The distribution
of continuous variables was used for normality. The data were
presented as mean+SD, except where otherwise specified. Rates
and proportions were analyzed by Fisher’s exact test and x2 test
of general association where appropriate. The data were checked
for normality using Kolmogorov Smirnov Z-test for individual
variables of all groups. Pearson product correlation was used
to assess for relationships among appropriate variables, two
sample student- t test with assumption of unequal variance
measured during 6MWT alone (age, sex, height, weight, body
mass index), distance ambulated, resting and exercise heart
rate, blood pressure, respiratory rate, oxygen saturation were
evaluated for their association with 6MWD by first univariate
analysis with the spearman’s correlation test and then adjusted to
multivariate analysis using stepwise multiple linear regression.
To determine entry and removal of candidate variables from the
model P-values of 0.05 and 0.01 were used respectively. Kaplan-
Meier method was used to compare patients by categories of
6MWD (<149- severe, 150-249 moderate, 250-349 mild, >350
normal). 6MWD measured in our study was compared with
predicted 6MWD derived from the studies of Enright PL &
Sherrill DL [3] for healthy adults.
Optimal reference equations
From healthy population based samples using 6MWD
methods are not yet available, several authors [1-16], determined
factors affecting 6MWD in healthy adults and proposes the
reference equation or normative data for 6MWT outcome (Table
1). When 6MWD is reduced a thorough search for the cause of
the impairment should be made i.e. PFT, Cardiac function, anklearm
index, muscle-strength, nutritional status, orthopaedic and
cognitive function.
Interpreting the results
Once 6MWD for a given patient is available we have calculated
the predicted distance using equation from published studies of
healthy people of same age group much like spirometry.
Result
Patient’scharacteristics
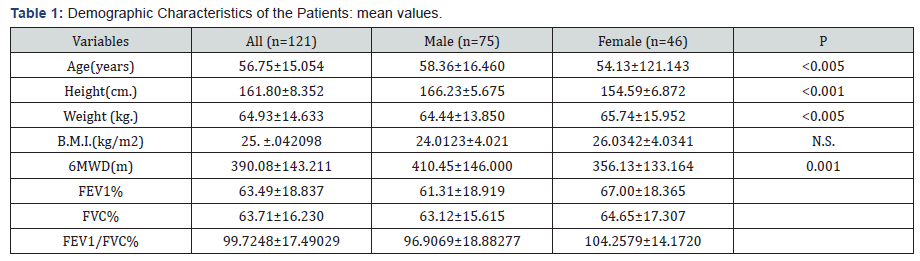
Table1 shows the physiological characteristics of the patients
and their relation with 6MWD. We evaluated 121 patients
between 13-85 years of age, 32 smokers. 108 had respiratory
disease, 12 had cardiac disease, most of the patients completed
the test. Mean age, height and weight were 56.75+15.054years,
161.80+8.352cm, 64.93+14.633kg respectively. Mean FEV1%,
FVC%, and FEV1/FVC% were 63.49+18.837, 63.7+16.230, and
99.72% respectively.
As per pulmonary function test
41(33.58%) patients had obstructive airways disease of
which 20 (18.2%) had mild, 16 (13.2%) moderate and 5 (4.1%)
had severe obstruction. 43 (35.53%) had restrictive disease of
which 27 (22.3%) had mild, 13 (10.7%) moderate, and 3 (2.5%)
had severe restriction.15 (12.40%) had combined obstructive
and restrictive disorder of which 3 (2.5%) had mild, 7 (5.8%)
moderate and 5 (4.1%) had severe disorder,22 (18.18%) had
normal spirometry. Mean 6MWD was 390.08+143.211m (range
264.769-533.29). 51 patients walked >400m, 24 between 300-
400m, 19 between 200-300m, 11 between 100-200m, and 2
patients walked <100 m.
a) In males: Total patients were 75, mean age, height
and weight were 58.36+16.460years, 166.23+5.675cm,
64.44kg+13.850 respectively. Mean FEV1%, FVC% and FEV1/
FVC% were 61.31+18.919, 63.12+15.615, 96.90%+18.88277.
6MWD was 410.45+146.000m (264.45-556.45).
b) In females: Total patients were 46, mean age,
height and weight were, 54.13+12.143yrs, 154.59+6.872cm,
65.74+15.952kg. Mean FEV1%, FVC% and FEV1/FVC% were
67.00+18.365, 64.65+17.30, 104.2579+14.01720 respectively.
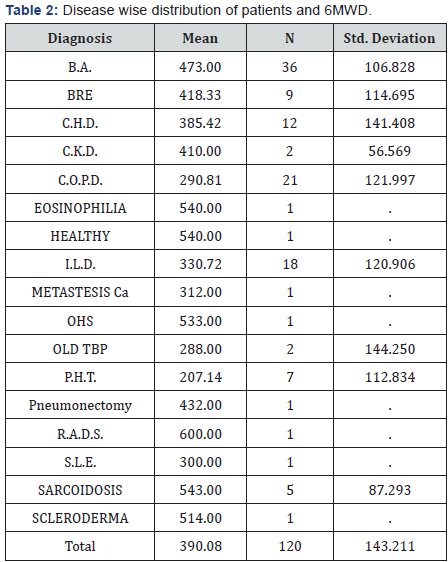
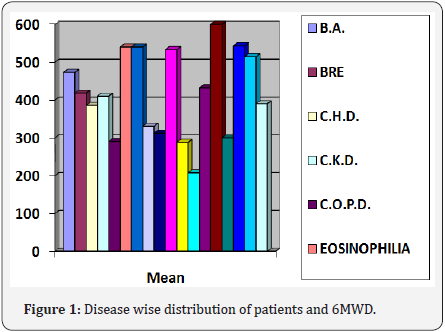
6MWD was 356.13+133.164m (222.966-489.294) 6MWD was
lower in females. Disease wise 6MWD (Table 2 & Figure 1) was
290.8+121.997m (89-411) in COPD, 207+112.834m (100-430)
in IPAH, 330.72+120.906 m (151-525) in ILD, 385.45+141.408
m (198-55)in CHF,473.00+106.828m (250-655) in BA,
418+114.698 m (146-655) in Bronchiectesis. 101 (83.40%)
patients completed 6MWT of which 31(30%) had to stop during
walking for few seconds but resumed walking, 20 (16.50%)
patients could not complete the test, and the test had to be
terminated the various reasons were breathlessness, giddiness,
fatigue, tiredness, chest heaviness, drop in saturation.
As per reference [6] 55 (46%) patients achieved lower limit
of normal (LLN), 15 (12.50%) achieved target walk distance.
Disease wise COPD 4(19%), ILD 8 (44.44%), PHT 2 (28.37%),
CHD 8 (90%), Sarcoidosis 4 (80%), Bronchiectasis 4 (44.44%)
and B.A. 22 (60%) patients achieved LLN.1 patient achieved
target walk distance in COPD, ILD 3 (16.66%), Sarcoidosis 2
(40%), PHT 1(14.30%), Bronchial Asthma 9 (24.32%) and
others 1(14.30%) could achieved target walk distance.
Correlation between 6MWD and various physiological and pulmonary parameters
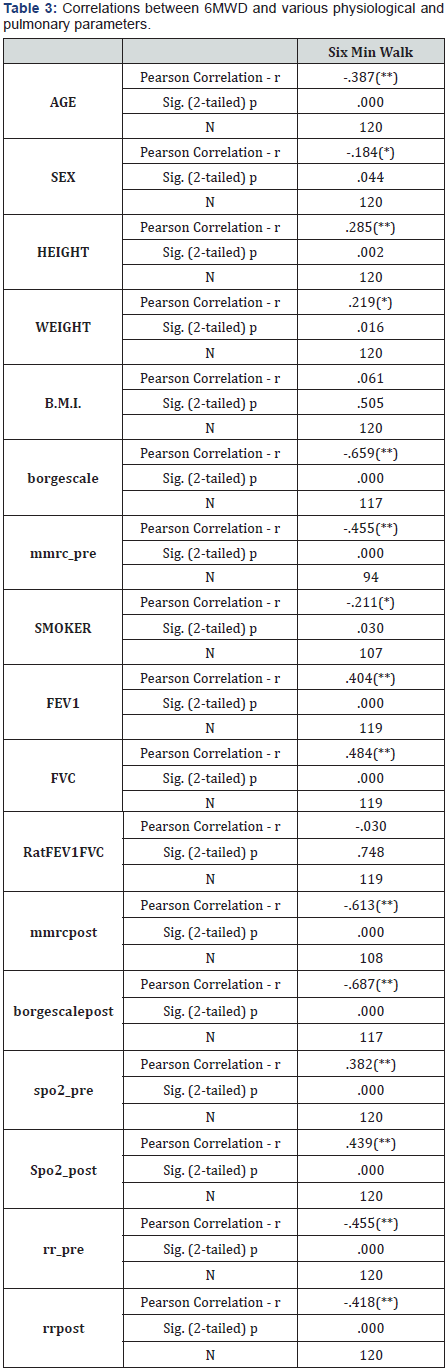
(Tabb 3) Male tend to be significantly taller and BMI less
than female. Significant positive correlation found between
6MWD and height (p<0.002, r-=o.285) and weight (p<0.016, r =
0.219), but no correlation was found between 6MWD and B.M.I.
Significant negative correlation found between age (p=0.000, r
=0.387), Borg score of dyspnoea, fatigue (p=0.000, r =0.659), and
MMRC score of dyspnea (p=0.000, r=0.455), (correlation was
more significant post-test for Borg and MMRC Score (p=0.000,
r=0.687 and p=0.000, r=0.613) and smoking (p<0.030, r=0.211).
Significant positive correlation found between spirometry
values FEV1% and FVC% (p=0.000, r=0.404, P=0.000, r=0.484
respectively) and SPO2 pre and post-test (p=0.000, r 0.382,
p=0.000, r=0.439 respectively.
Discussion
The ability to walk for a distance is an easy way to
measure exercise capacity in patients with cardiac-pulmonary
diseases. 6MWT is found to be an effective way of assessing
exercise tolerance. We evaluated 121 adults, mean 6MWD was
390.80+143.211m, males cover more distance than females.
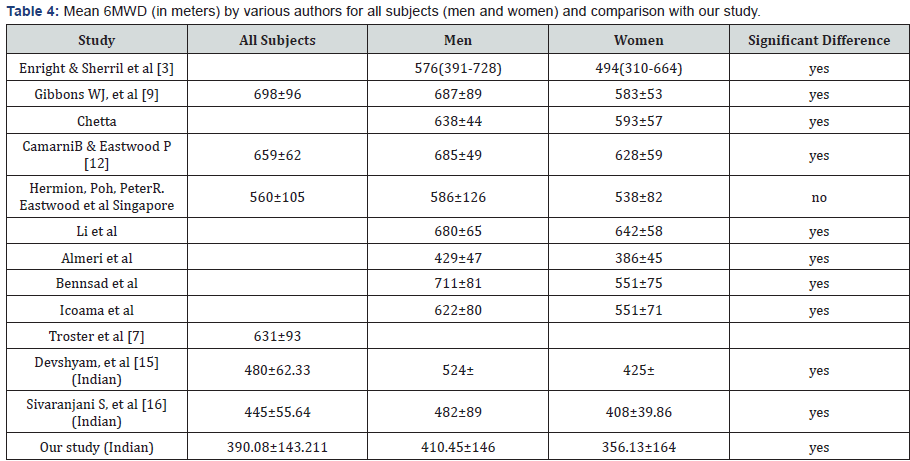
We compared 6MWD with several studies done world over in
healthy adults1-16 (Table 4). A reference equation published
by Enright & Sherril [3] found that age, gender height, and
weight were independent factor associated with 6MWD. They
administered 6MWT to 117 healthy man and 173 healthy
women aged 40 to 80 years, the median distance walked was
576 m for man and 494 m for women. We selected this reference
[3] equation for computation of 6MWD in our study: For Men:
6MWD= (7.57x height in cm)-(5.02x age in yrs.)-(1.76xwt.)-309,
alternative using B.M.I 1140m-(5.61X B.M.I.)-(6.94x age). For
women: 6MWD= (2.11x height in cm) – (2.29 x wt. in kg) - (1.76x
age in yrs.)+667, alternative using B.M.I.: 1017m–(6.24x B.M.I.)–
(5.85x age in years) when using either equations we subtracted
153 m for men and 139 m for women as lower limit of normal
(LLN). In our study mean 6MWD was 390+143.211m. The mean
6MWD values described in various studies1-16, was 613+93m
and 659+62m in western and Caucasian healthy subjects
respectively, compared to above studies our results were 62%
(lower by 38% than western studies).There are two studies
done in Indian healthy adults: Devshyam, et al [15] (281 healthy
subjects mean 6MWD was 480+62.33m), and Sivaranjani SS,
et al [16] (60 healthy subjects mean 6MWD was 445+55.64m
) compared to these two studies our mean 6MWD were 82%
and 87% lower by 18% and 13% respectively. Al Ameri [17]
studied 129 Saudi Arab subjects, mean 6MWD was 341+70
m, compared to our study it was significantly lower, marked
difference in above study may be due to selection of the patients, (COPD (37%), PHT (1%), ILD (62%)). In our study we selected
all types of patients, when calculated for COPD, ILD, PHT, 6MWD
was 283m which is lower by 18%. In our study mean 6MWD
value in male and female patients were 410.45+146.000 and
356.13+133.164m respectively. Compared to study done by
Paul Enright & D Sherril [3] (6MWD in healthy adult males and
females, mean 6MWD were 576m and 494m respectively), our
mean 6MWD values were 71.17% (29% lower) in males and
72% (28% lower) in females respectively. In comparisons to
study done by: (1) Devshyam, et al. [15] (mean 6MWD were 524
and 425m in males and females), our study showed significant
lower value of 6MWD [410m (78.84%) and 356m (76%), lower
by 22% and 24%]. (2) S. Sivaranjani S, et al [16] (6MWD were
482+45.89 and 408+29.86m in males and females respectively),
our study showed lower values of 6MWD [410 m (85.41%)
and 356 m (87.24%) lower by 15% and 13% respectively]. In
our studied population the 6MWD has a significant correlation
with various physiological and pulmonary parameters (Table
4). Positive correlation found with height (p<0.002, r=0.285,)
and weight (p<0.016, r=0.219). Significant negative correlation
found with gender (p<0.044, r=0.184 males covered more
distance than females, normal reference values are lower in
females than males) and age (p=0.000, r=0.659). 6MWD was
positively correlated with FEV1 (p=0.000, r=0.404), FVC%
(p=0.000, r=0.484) and oxygen saturation pre and post (p=0.000,
r=0.382, p=0.000, r=0.439 respectively). 6MWD decreases with
decrease in FEV1, FVC and SPO2, and inversely correlated with
Borg score of dyspnea (p=0.000, r=0.659) and MMRC Scale
(p=0.000, r=0.455) of dyspnea, as the age, Borg and MMRC scale
of dyspnea increases 6MWD decreases, also smoking (p<0.300,
r=0.211) decreases the 6MWD.
Disease Specific Discussion (Table 5)
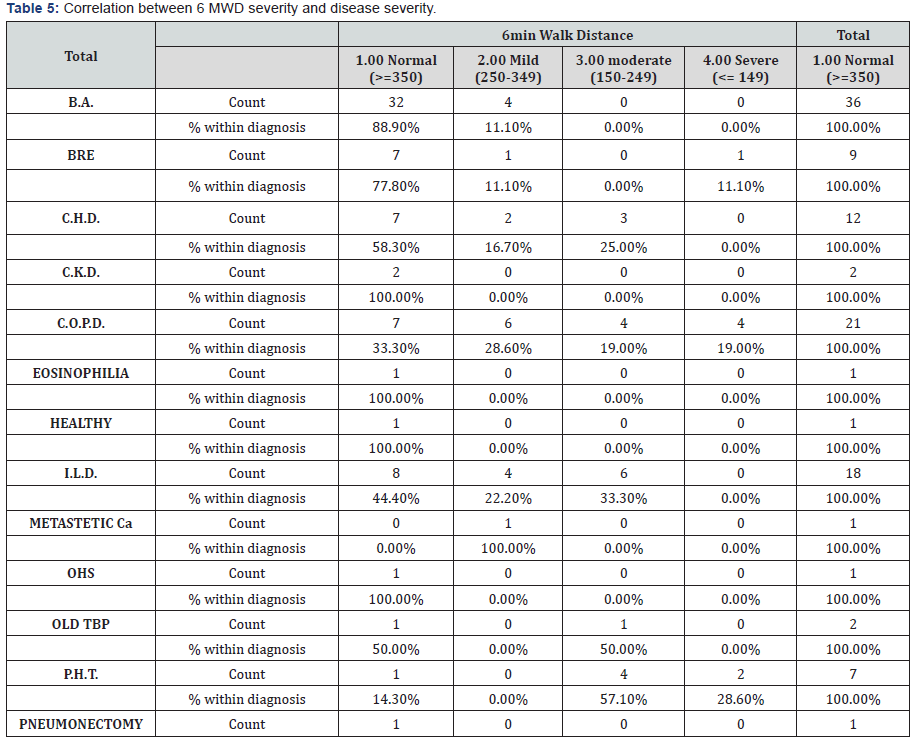
COPD: The FEV1 is often used to grade the severity of disease;
however patients with COPD have systemic manifestations
that are not reflected by the FEV1%. Several factors have been
identified that predict poor survival in COPD these includes low
FEV1, active smoking, hypoxemia, poor nutrition, presence of corpulmonale,
resting tachycardia, lower exercise capacity, severe
dyspnea, poor health related quality of life, anemia, frequent
exacerbations, co-morbid illness, and low DLCO. Patients with
FEV1 <35% predicted have about 10% mortality per year, if
patient reports that they are unable to walk 100 meters without
stopping because of breathlessness, the 5-year survival is only
30%. A multidimensional prognostic index [17] that takes into
account several indicators of COPD prognosis are the BODE
Index. Inclusion of 6MWD along with FEV1, dyspnea rating and
BMI into a 10-point index was better at predicting mortality
in COPD than FEV1 alone. B.R. Celli, Cote C.G., JM Martin et al.
[18] evaluated 207 patients and found that above four factors
predicted the risk of death in this cohort: in which a higher score
indicates a higher risk of death. The hazard ratio (HR) for death
from any cause increased by 1.34 per point increase in BODE
INDEX (95% confidence interval 1.26 to 1.42, p<0.001) and HR
for respiratory cause was 1.62 (95% confidence interval-1.48 to
1.77, p<0.001). “0” point is given for 6MWD >350 m, 1point for
250-349 m, 2 points for 150-249 m, and 3 points for <149 m.
This demonstrate the independent role that exercise capacity
measured by 6MWT has in predicting mortality in COPD. In our
study we had 21 patients of COPD 18 male (all were smokers),
3 female (non-smokers), mean 6MWD was 290.81meters (range
89 to 401 meters), 9 patients could not complete 6MWT due
to dyspnea, fall in saturation, only one patient could achieved
Target 6MWD (100%), as per ref 6 equation 3 patients could not
achieve lower limit of normal distance walk, 4 patients walked
<149 meters only (3 points), 4 patients walked between 150-
249 meters (2 points), 6 patients walked between 250-349
meters (1 point) and 7 patients walked > 350 meters (0 point).
As per BODE INDEX: 2 patients had score of “10”, 2 patients had
score of “9”, 1 patient had score of “8”, 5 patients had score of
“7”, 2 patients had score of “5”, 9 patients had score of “2-4”. A
BODE score > 7 is associated with 30% 2 years’ mortality, where
as a score of 5-6 is associated with 15% 2 years’ mortality,
if BODE score is<5 the 2 years’ mortality is less than 10%. In
our study 10 patients had BODE score of >7, 2 patients had
score of 5, and 9 patients had score<5 that can predict 2 yrs.
mortality, which is higher in 12 patients in our study. In another
study done by Szekely LA, et al [19] they evaluated 47 subjects
preoperatively for LVRS a 6MWD <200 meters had a specificity
of 84% for prediction of 6 months mortality after LVRS for
emphysema. Patients with unacceptable risk for this procedure
were identified by the 6MWT and a resting PCO2>45 mmHg. In
our study 6 patients walked < 200 meters which is significant.
In a study done by Casanova C, Cote C, JM Martin, et al. [20] for
576 COPD patients with wide range of airflow obstruction seen
at 4 centers in two countries reported on the value of 6MWD and
Spo2 during 6MWT, 6MWD was a good independent predictor
of all cause and respiratory mortality particularly for the group
with FEV1<50% of predicted and fall in Spo2>4% or to < 90%.
In our study 11 patients had FEV1 <50% with 10 patient’s
6MWD <350m with fall in saturation >4% during exercise test
(Spo2<90%). In a mixed group of patients with advanced lung
disease undergoing evaluation for lung transplantation a study done by Kadikar A, [21] many of had severe COPD, 6MWD was
<300 meters had a 80% mortality rate. In our study we have
9 patients who had severe COPD 5 walked < 300m another 5
patients who had combined obstructive and restrictive disorder
walked <300 meters, in all these patients 6MWD predicts higher
mortality.
Idiopathic Pulmonary Arterial Hypertension: In patients
with Idiopathic pulmonary hypertension 6MWD was significantly
but modestly related with New York Heart association functional
class, baseline cardiac output, pulmonary vascular resistance,
but not mean pulmonary artery pressure. A study done by
Shoichi Miyamoto, John Satohet, et al [22] in 43 patients with
pulmonary hypertension together with echocardiography, right
heart catheterization and measurement of plasma epinephrine
and norepinephrine. Symptom related cardiopulmonary
exercise performed in a sub sample of patients (n=27) distance
walked in 6 minutes was significantly shorter in patients than
in age and sex matched subjects (297+188 versus 655+91m,
p<0.001). The distance walked had strong significant correlation
with CPET parameters. Among the various parameters only
6MWD <332 meters independently related to mortality by
multivariate analysis. Patients had a lower survival than those
walking further. In our study we had 7 patients of pulmonary
hypertension out of which 5 patients walked <250 meters and
2 walked < 140 meters, indicating higher mortality. In another
study done by Paciocco G, et al [23] 6 MWD <300 meters and
reduction of saturation >10% at the end of 6MWT was associated
with increased mortality with an HR of 2.4 and 2.9 respectively.
In our study 7 patients of pulmonary hypertension 5 patients
walked < 300m with 2 patients desaturases >10% at the end of
the test which is quite significant.
Idiopathic Pulmonary Fibrosis: The importance of
measuring oxygen desaturation during 6MWT was highlighted
in a study of patients with IPF by Flaherty KB, et al [24] which
showed that a decrease in SPO2 during exercise had prognostic
value though ATS does not recommends measurement of SPO2
during test, 6MWD was a weak predictor of mortality which was
no longer significant when patients were split into presence or
absence of SPO2< 88% during exercise. Patients with an SPO2<
88% during their 6MWT had a median survival time of 3.2 years,
compared to 6.8 years in those with lesser degree of oxygen
desaturation. Even in those with a milder degree of desaturation,
a 10-point increase in desaturation area gave HR for mortality of
1.33 (95% confident interval, 1.08 to 1.63 p=0.007). For patients
with baseline 6MWT SPO2< 88% the best predictor of mortality
was serial decrease in diffusion capacity of carbon mono-oxide
[25]. In those with lesser degrees of 6MWT desaturation at
baseline serial decrease in FVC and increase in desaturation
significantly predicted mortality. In our study 12 patients’
desaturases > 4% (range 4 to 9%) (base line spo2 <88%). This
finding highlights the importance of measurement of spo2
during 6MWT to assess prognosis, an approach specifically
not recommended by ATS. In our study 3 patients could not complete the 6MWT due to severe dyspnea, tachypnea, and drop
in saturation >4%, 15 patients completed 6MWT, 8 stopped
due to dyspnea and drop in SPO2 >4% for 15-30 seconds but
continue walking after rest. In another study by Vibha N Lama
et al [26] prognostic value of desaturation during 6MWT in IPF
patients, exercise induced hypoxia is an index of the severity of
ILD. Desaturation during 6MWT predict mortality for patients
with UIP (n=83) and NSIP (n=27), desaturation is defined fall in
saturation < 88% or less during 6MWT. Patients desaturated had
higher mortality than those who did not have.
Chronic heart failure: 12 patients (9 males, 3 female) mean
6MWD is 385.42+408 m, 2 patients could not complete the test
due to drop in saturation >4%, 5 patients could not achieve
lower limit of normal walk distance. 2 patients achieved Target
walk distance. In patients with CHF strong correlation between
6MWD and exercise ergometry and VO2 max were observed by
several researchers and moderate to strong association with
NYHA functional classification. Results of other studies in the
same population have shown that distance walked in 6MWT
(<300m) can identify those with increased likelihood of death
or hospitalization within a time frame ranging from 3 months to
1 year. In our study 5 patients walked < 300 m out of which only
one could achieve lower limit of normal 6minute walk distance.
In a study done by Lipkin DP, et al [27] 26 patients with mean
age of 58 years (range 36-58) with stable CHF NYHA class II &
III and 10 normal subjects of similar age there was significant
difference in walking distance between normal, CHF patients
with class II & III (683, 558, and 402m) respectively, the distance
walked varies with oxygen consumption. In a study done by Shah
MR, et al [28] in patients with congestive heart failure (CHF)
those with a 6MWD below a median of 218 m had a 4-6-fold
higher mortality risk for every 100 m decrease in 6MWD, the HR
for death, hospitalization and the composition of the two end
points was o.58, o.85 and 0.75 respectively. In another CHF study
done by Passantino A, et al [29] 6MWD and short term change
in 6MWD in response to change to therapy were significant
independent predictor of survival. Prognostic value of 6MWT
in stable CHF patients a study by Sakir Arslam et al [30] with
two groups of patients, death risk was higher in patients with
a distance of <300m (p=0.05) with LVEF<0.30(p=0.02). Studies
of Left Ventricular Dysfunction (SOLVED) was the first large
investigation (898 patients) by Bittener, et al [31] to show a
strong correlation between distance walked during 6MWT and
death (decrease in distance walked increases the mortality).
In our study 5 patients walked <300m. with drop in saturation
showed increased mortality.
Bronchiectasis: Total 9 patients (5male, 4female) 2patients
could not complete the test due to drop in saturation, tachypnea,
and dyspnea, 4 patients could not achieve lower limit of normal
distance, 8 patients could not achieve Target walk distance,
4 patients had > 4% drop in saturation. In a study by Lee A31
6MWD severity of disease and HRQOL had a stronger association
compared to physiological measures of disease severity.
Sarcoidosis: 5 patients with mean 6MWD-543.0 +87.293m
all patients walked > 400m and achieved lower limit of normal
walk distance, only one patient achieved Target walk distance,
all had > 4% drop in saturation during 6MWT but all completed
6MWT, 3 patients became tachyponic with respiratory rate>24/
mt. In a study done by Bittener, et al [31] for 26 Saudi patients
with pulmonary sarcoidosis all completed 6MWT female covered
shorter distance than males, lowered Spo2 at end of test than
others, mean 6MWD for entire cohort was 364m, females < than
males [343m (223-389) vs 416m (352-500m), with significant
lower Spo2 at end of 6MWT than male [90.5% (61-99%) vs
96% (75-98%). In our study there was no such difference seen
in distance walked in 6 minutes but all patients had drop in
saturation >4% which is significant [33-36].
Bronchial Asthma: 37 patients (18 male, 19 female), 1had
severe, 7 moderate, 14 mild, 15 patients had normal disease, all
had completed 6MWT, 8 male and 4 female became tachyponic
with 8 had >4% drop in saturation, 33 patients walked >350 m, 4
walked between 150-249m, 10 patients could not achieved lower
limit of normal (LLN) as per reference equation, all had long
standing Bronchial Asthma.In a study done by AL Ameri35 for
respiratory disease patients 6MWD was significantly correlated
with FEV1 patients.
Other patients: (1Carcinoma lung, 2RADS, 1Tuberculosis,
2CKD, 1Pneumonectomy all patients completed the test except
1T.B. patient), 5 walked >350m, 1 between 250-349 m, 1<249m
(150-249).
In our study we demonstrated that 6MWT can be safely
performed. Its validity reliability, and reproducibility were
studied in several populations world over [1-16]. As per our
knowledge this is one of the study done in Indian population,
with no untoward events or complications that required
emergency management, was highly tolerable in different
age groups, gender and in patients with advanced cardiacrespiratory
conditions, only few patients could not complete the
test. 6MWD is a useful marker for the severity and progression
of the disease. The co-relation of 6MWT and PFT, in patients
with respiratory diseases makes this test easy and simple tool
for assessing the disease status. 6MWD was lower in females
and had significant positive correlation with height, FEV1, FVC,
SPO2, and negative correlation with age, Borg and MMRC scale
of dysponea and smoking.
All the authors designed the study, review the case, revised
and checked it. PKV wrote the manuscript, prepared tables and
images, reference collection, and obtained informed consent
from the patient. PSB and GBG helped smooth conduction of the
test, helped in writing manuscript. SVR consultant Respiratory
Physician reviewed draft, supervised whole procedure suggested
improvements. JRS, HOD helped in conducting, selection of place,reviewed draft, RSM helped in preparation of draft, suggested
reviews and references.
Our sincere thanks to Dr. A.S. Chitnis Senior pulmonologist
and D.N.B. Teacher for his technical guidelines and help provided.
We are also thankful to the staff of pulmonary and physiotherapy
department, to the management of Jaslok Hospiatl to allow us to
conduct this study and to all the participants.
To know more about Open Access International
Journal of Pulmonary & Respiratory Sciences please click on: https://juniperpublishers.com/ijoprs/index.php


Comments
Post a Comment