Effectiveness of Mhealth to Increase Cervical Cancer Screening: Systematic Review of Interventions-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS INTERNATIONAL JOURNAL OF PULMONARY & RESPIRATORY SCIENCES
Abstract
Background: Estimated one
million-plus women worldwide are currently living with cervical cancer.
Many of them have not any access to health services for prevention,
curative treatment or palliative care. Cervical cancer is a consequence
of a long-term infection with human papillomavirus (HPV), and the
majority of cervical cancer cases (>80%) are currently found in low-
and middle-income countries. In fact, an increasing body of literature
indicates that HIV-positive women have an increased risk of developing
cervical cancer in comparison with their HIV-negative counterparts.
Cervical cancer is most notable in the lower-resource countries of
sub-Saharan Africa as the result of the highest incidence of
HIV-infected women.
Pilot mHealth projects have shown that, particularly
in developing countries, mobiles phones improve communication and
information-delivery and information-retrieval processes over vast
distances between healthcare service providers and patients. Mobiles
phones provide remote access to healthcare facilities, facilitate
trainings for, and consultations among health workers, and allow for
remote monitoring and surveillance to improve public health programs
awareness.
mHealth interventions can potentially influence
health-related behavior (and, in turn, health outcomes) via effecting
changes in mediators of behavior change such as knowledge, attitudes,
community peer norms, beliefs and self-efficacy. SMS can be customized
to fit the needs of specific individuals by delivering tailored messages
that are more likely to catch the individual’s attention and be
perceived as personally relevant and interesting.
This systematic review will investigate whether mHealth interventions could improve cancer screening uptake in risk women.
Objective: To assess the
effectiveness of different mHeath (SMS, calls, letters and emails
reminders) interventions to improving cervical cancer screening in risk
women.
Search methods: We searched for
studies in MEDLINE, Scorpus, PsychINFO, Cochrane Central Register of
Controlled Trials (CENTRAL), CINAHL, World Health Organization Global
Health Library regional index, Mobile Active http://
www.mobileactive.org, Web of Science and Grey literature. In addition,
hand-searching was performed for the original published version of this
review, but not for this update. Issues of the following journals will
be hand-searched: AIDS, AIDS Care, Health Education Journal, Health
Psychology and Journal of the American Medical Association
Selection criteria: We included the
following studies design: randomized control trials, quasi-experimental
studies and non-randomized control trials assessing different mHealth
interventions in improving cervical cancer screening outcomes.
Data collection and analysis: Two
reviewers independently (JT and LM) identified and critically appraised
all included studies. Study design, characteristics of study
populations, interventions, controls and study results were extracted by
two review authors. In addition, the risk of bias of included studies
was assessed independently by two reviewers. We interpreted the results
from meta-analysis. We reported the odds ratio with 95% confidence
intervals for the different outcomes.
Main results: We found 4731 studies
in different electronic databases, 3004 studies were included after
removing duplicated studies. Among them, 79 studies were fully assessed
and then, 51 were excluded and 28 studies were assessed for eligibility
criteria. 11 studies were excluded with reasons and 17 studies were
included in meta-analysis. The overall results revealed that call
reminders increased 44% of cervical cancer screening compared to the
standard care, with p-value of0.01. 8 studies were included in this
meta-analysis and the total number of participants was 29477. Call
reminders improved 89% of cervical cancer screening adherence, with
highly statistical results (Test for overall effect: Z = 5.23, P <
0.00001). 3 studies and 1340 participants were included. Lastly, letter
reminders improved 20 % of cervical cancer screening compared to the
standard care. 8 studies and 345835 participants were found in the
overall results. Therefore, this result was not statistically
significant (P=0.15).
The effect of call reminders on cervical cancer
screening and its adherence was high; therefore the impact of letter
reminders on cervical cancer was moderate.
Authors’ conclusion: This systematic
review supports the use of call reminders in improving cervical cancer
screening and adherence to testing. The main outcomes were graded as
high level of evidence. Then, call reminders could be suggested to be
encompassed in different national policy in screening cervical cancer in
risk populations. The lack of sufficient evidence on the subject limits
the reliability of the current cervical cancer screening guidelines for
high risk women is the leading cause of diagnosing cervical cancer in
the last stage. Further studies in this field will provide the sole for
preventing cervical cancer. However, this review could orientate public
health policy makers.
Background
Description of the condition
An estimated one million-plus woman worldwide is currently
living with cervical cancer [1]. Many of them have not any access
to health services for prevention, curative treatment or palliative
care [1]. Cervical cancer is a consequence of a long-term infection
with human papillomavirus (HPV), and the majority of cervical
cancer cases (>80%) are currently found in low- and middleincome
countries [1].
Nowadays, Cervical cancer constitutes a major health problem
worldwide [2]. Recent studies have demonstrated cervical cancer
is the leading cause of female cancer mortality and second most
common cancer in women worldwide [3] and It is responsible for
528,000 new cases of cancer and causes 270,000 deaths each year
(WHO 2012) [4]. Several demographic, economical and behavioral
risk factors have been studied in relation to cervical cancer [5].
Most of them may influence the risk of cancer through their
effects on the risk of HIV and HPV infection Ali-Risasi [5]. Different
studies have shown that HIV infection has been associated with an
increased risk of cervical cancer Kumakech [6]. Epidemiological
studies have clearly established human papillomavirus (HPV)
infection as the main cause of cervical cancer. In most studies,
HPV16 and HPV18 are the predominant genotypes: they cause
about 70 % of precancerous lesions and cervical cancer [7,5]. In
Sub- Saharan Africa however, other oncogenic genotypes have
been reported 5,8,9,10]. In fact, an increasing body of literature
indicates that HIV-positive women have an increased risk of
developing cervical cancer in comparison with their HIV-negative
counterparts [11,12]. Sub-Saharan has the highest incidence of
HIV-infected women, and then cervical cancer is most notable in
the lower-resource countries of sub-Saharan Africa [4]. In sub-
Saharan Africa, 34.8 new cases of cervical cancer are diagnosed
per 100 000 women annually, and 22.5 per 100 000 women die
from the disease [4]. Compared to North America where there are
6.6 new cases of cervical cancer diagnosed per 100 000 women
annually, and 2.5 per 100 000 women die, Sub-Saharan Africa
has 34.8 and 22.5 per 100 000 respectively [4].With increasing
attention to cervical cancer prevention in developing countries
[13], several pilot screening programs have been initiated
throughout sub-Saharan Africa Rosser [14]. The World Health
Organization (WHO) recommends a more aggressive cervical
cancer screening [15].
In fact, among all malignant tumours, cervical cancer is the
one that is most easily preventable by screening Arbyn M [16].
The detection of cytological abnormalities by microscopic
examination of “Pap smears”, and the subsequent treatment
of women with high-grade cytological abnormalities, avoids
development of cancer [16,17]. With increasing attention to
cervical cancer prevention in developing countries, several pilot
screening programs have been initiated throughout sub-Saharan
Africa [14]. Therefore, some challenges are associated with
screening, ranging from low levels of cervical cancer screening due
to poor access to organized screening, a lack of or low information
on cervical cancer screening, stigma, women’s perception of low
threat of disease and overburdened health care facilities which
lack equipment and are understaffed [18,19].
Description of the intervention
Mobile telecommunication technologies into the health
arena is also known as mobile health, mHealth or eHealth [20].
Mobile phone technology is increasingly viewed as a promising
communication channel that offers the potential to improve health
care delivery and promote behavior change among vulnerable
populations [20].
Pilot mHealth projects have shown that, particularly in
developing countries, mobile phones improve communication and
information-delivery and information-retrieval processes over
vast distances between healthcare service providers and patients
[21,22]. Mobiles provide remote access to healthcare facilities,
facilitate trainings for, and consultations among, health workers,
and allow for remote monitoring and surveillance to improve
public health programs. This phenomenon has the potential to
lead to an overall increase in the efficiency and effectiveness of
under-resourced health infrastructures, ultimately translating
into benefits for patients [22].
SMS-based interventions enable patients and providers to
‘‘interact’’ via two-way communication. To date, this feature has
been implemented in various ways. For example, most studies
have used systems to automate the message delivery process for
providers, ranging from fully automated clinical appointment
reminders [23] to staff developing and delivering the messages
themselves. SMS interventions also have enabled patients to
communicate with providers to confirm thier adherence to any
health interventions or outcomes [24,25]. Other studies have
mixed SMS, call, email and letter reminders to improve health
related outcomes. In fact, letter reminders could be used in
network inaccessible areas or cellphone deprived women.
The use of mHealth to improve health related outcomes is
receiving more attention in public health as emerging evidence
suggests reminder messages, call, email and letter can improve
several health outcomes.
How the intervention might work
Individual and cultural factors, such as stigma, isolation,
symptoms of illness, and psychological distress [26-28] may
contribute then to non-adherence of cervical cancer screening.
mHealth interventions can potentially influence healthrelated
behavior (and, in turn, health outcomes) via effecting
changes in mediators of behavior change such as knowledge,
attitudes, community peer norms, beliefs and self-efficacy [29].
SMS can be customized to fit the needs of specific individuals by delivering tailored messages that are more likely to catch the
individual’s attention and be perceived as personally relevant
and interesting [30]. Then, mHealth plays an active role in one’s
health and medical care leads to better healthcare quality, better
clinical health outcomes, and likely lower healthcare costs [31].
Interventions aimed at increasing patient involvement have
shown beneficial effects on satisfaction and functional status
[32,25], quality of life [33], perceived control over cervical cancer.
Why it is important to do this review
Studies have shown that well-organized cytological
screening at the population level, every three to five years,
and the incidence of cervical cancer can be reduced up to 80%
[34,16]. Furthermore, the vaccination against the most common
oncogenic human papillomavirus (HPV) types, HPV-16 and HPV-
18, could prevent development of up to 70% of cervical cancers
worldwide [35]. Therefore, this vaccine is quite inaccessible in
developing countries; by the way, the Pap smear reminds the
cornerstone of cervical cancer screening in developing countries.
Then, improving cervical screening through different behavioral
intervention is the only way that could decrease drastically the
morbidity and mortality of cervical cancer.
Eight studies exploring reasons women did not utilize cervical
cancer screening were included. Women in Sub-Saharan Africa
reported similar barriers despite cultural and language diversity
in the region [36]. Women reported fear of screening procedure
and negative outcome, low level of awareness of services,
embarrassment and possible violation of privacy, lack of spousal
support, societal stigmatization, cost of accessing services and
health service factors like proximity to facility, facility navigation,
waiting time and health care personnel attitude [36].
This systematic review will investigate whether mHealth
interventions could improve cancer screening uptake in risk
women.
Objectives
To assess the effectiveness of different mHeath (SMS, calls,
letters and emails reminders) interventions to improving cervical
cancer screening in risk women.
Methods
Criteria for considering studies for this review
Types of studies
- Randomized control trials
- Quasi-experimental studies
- Non randomized control trials
4.3. Types of participants
Women at risk of developing cervical cancer
Types of interventions
SMS reminders
- Call reminders
- E-mail reminders
- Letter reminders
Types of outcome measures
Primary outcomes- Pap smear uptake
- Adherence to test pap smea
Proportion of abnormal pap smear
Search methods for identification of studies
(Cellular phone) OR (telephone) OR (mobile phone) OR (text
messag*) OR (testing) OR (short messag*) OR (cell phones) OR
(SMS) OR (short message service) OR (text) OR (mobile health)
OR (telemedicine) OR (health) OR (health communication) OR
(health education) OR (behavior) OR (ehealth)
(Uterine Cervical Neoplasm) OR (Cervical Neoplasms)
OR (Cervical Neoplasm) OR (Cervix Neoplasms) OR (Cervix
Neoplasm) OR (Cancer of the Uterine Cervix) OR (Cancer of the
Cervix) OR (Cervical Cancer) OR (Uterine Cervical Cancer) OR
(Cancer of Cervix) OR (Cervix Cancer)
(Test, Papanicolaou) OR (Pap Test) OR (Test, Pap) OR (Pap
Smear) OR (Smear, Pap) OR (Papanicolaou Smear)
(Randomized controlled trial) OR (controlled clinical trial)
OR (randomized controlled trials) OR (random allocation) OR
(double-blind method) OR (single-blind method) OR (clinical
trial) OR (trial) OR (clinical trials) OR (clinical trial) OR (singl*
OR doubl*) OR (trebl* OR tripl*) AND (mask* OR blind*) OR
(placebos) OR (placebo*) OR (random*).
Electronic searches
We searched for studies in:
MEDLINE
- Scorpus
- PsychINFO
- Cochrane Central Register of Controlled Trials (CENTRAL)
- CINAHL
- World Health Organization Global Health Library regional index
- Mobile Active http:// www.mobileactive.org
- Web of Science
- Grey literature
Hand-searching was performed for the original published
version of this review, but not for this update. Issues of the
following journals was hand-searched: AIDS, AIDS Care, Health
Education Journal, Health Psychology and Journal of the American
Medical Association.
Data Collection and Analysis
Selection of studies
Inclusion criteria was applied to all titles and, where available,
abstracts identified from the literature search by two review
authors. Potentially relevant references was then retrieve for
further screening by one review author and check by a second.
Any disagreement was resolved through discussion with recourse
to a third review author when necessary.
Data extraction and management
The following data were extracted:
- Author and year of publication
- Country, town, Setting
- study design
- Total number of intervention groups
- Unit of data analysis
- Sample size calculation
- Duration of follow-up
- total number enrolled
- Eligible participants
- Age
- Ethnicity
- Intervention details: type of intervention, description of intervention, frequency and duration of intervention
- comparator group(s)
- Outcomes measures
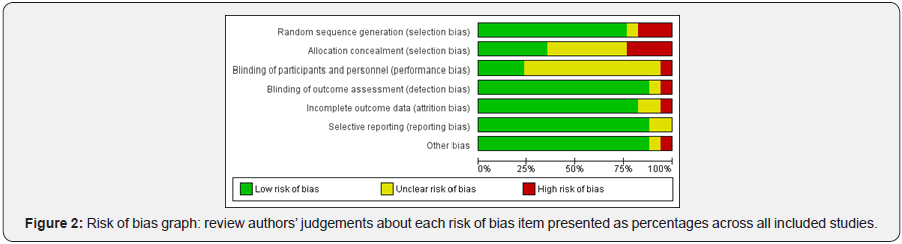
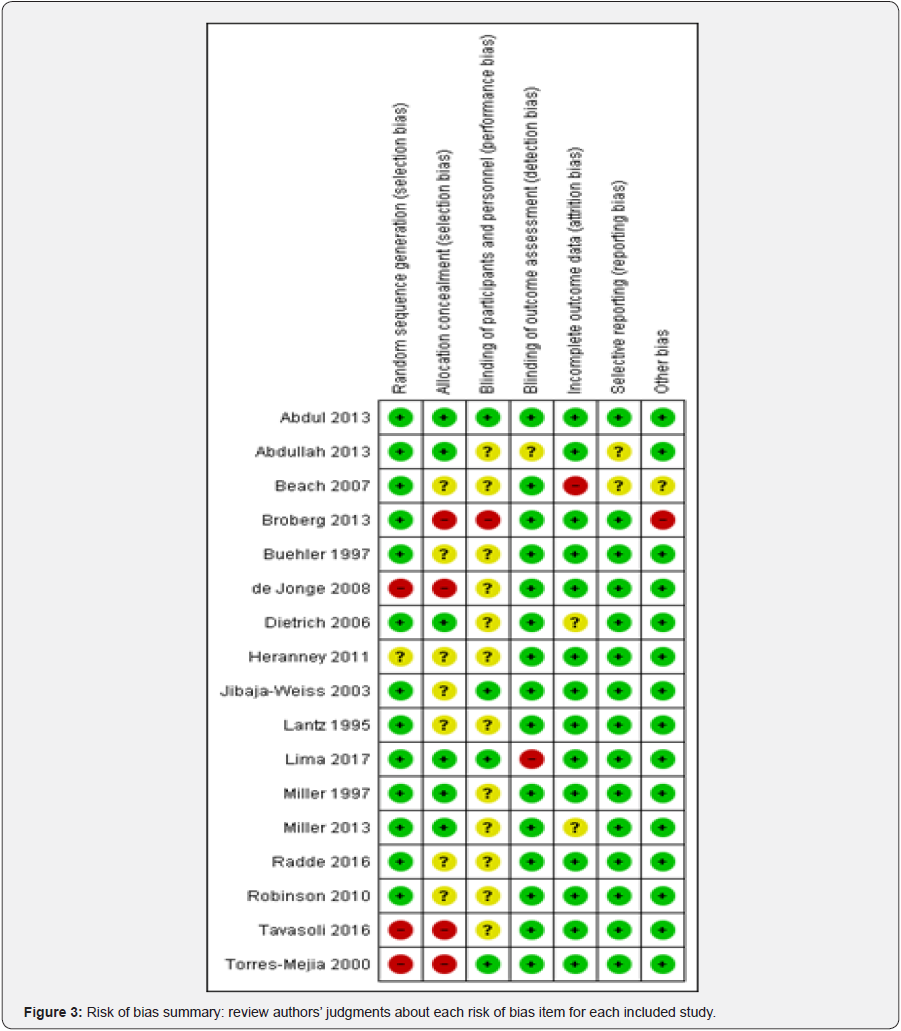
Risk of bias assessed in included studies using the Cochrane
Collaboration’s Risk of Bias tool. The tool includes the following
domains: random sequence generation; allocation concealment;
blinding of participants and personnel; blinding of outcome
assessment; incomplete outcome data; selective reporting; and
other sources of bias. Any disagreement will be resolved by
consensus, by consulting a third author.
Measures of treatment effect
We used only dichotomous outcomes we used the odds ratio
and its 95% CI was calculated.
Unit of analysis issues
The unit of analysis was individuals. After adjustment for
possible confounding, data derived from cluster-randomized
controlled trials produced same results. We included clusterrandomized
trials in the meta-analysis along with individuallyrandomized
trials. We adjusted for design effect using an
‘approximation method’.
Dealing with missing data
We did not experience any missing data in this systematic review
Heterogeneity between trials was assessed by visual
inspection of forest plots, by estimation of the percentage of I2
between trials which could be ascribed to sampling variation, by
a formal statistical test of the significance of the heterogeneity
and, if possible, by sub-group analyses. If we find substantial
heterogeneity, the possible reasons for this was investigated and
reported.
Funnel plots corresponding to meta-analysis of the primary
outcome was examined if we have 10 or more studies. We then
assessed the potential for small study effects. If there is evidence
of small-study effects, publication bias was considered as only
one of a number of possible explanations. If these plots suggested
that treatment effects may not be sampled from a symmetric
distribution, as assumed by the random effects model, sensitivity
analyses was carried out using fixed effects models.
Data synthesis was based on the heterogeneity of the studies.
When heterogeneity was not too large, we performed a metaanalysis.
In the presence of homogeneity, we used a fixed-effect
model for the meta-analysis. In the case of moderate or high
heterogeneity, we used a random-effects model to produce the
overall results.
Results
Results of the search

Seventeen studies were included in this systematic review
(see annex tables: Characteristics of included studies). Twelve
RCTs [2,37-47], two cluster randomized control trials [48,49], two
quasi-randomized control trial [50,51] and one non randomized
control trial [52].
Excluded studies
Ten studies were excluded from the review among which [53-
62] (see annex tables: Characteristics of excluded studies)
Risk of bias in included studies
Allocation (selection bias)
Allocation concealment was minimized in Abdul [37];
Abdullah F [48]; Dietrich [40]; Lima [51]; Miller [44]; Miller [2];
Radde [45]. In Beach [49]; Buehler [39]; Heranney [41]; Jibaja-
Weiss [42]; Lantz [43]; Robinson [46], selection bias was unclear,
therefore high in Broberg [38]; de Jonge [50]; Tavasoli [52];
Torres-Mejia [47].
Blinding (performance bias and detection bias)
Bias assessment stool revealed that performance bias was
reduced in Abdul [37]; Abdullah [48]; Lima [51]; Jibaja-Weiss [42];
Torres-Mejia [47]. unclear Beach [49]; Buehler [39]; de Jonge [50];
Dietrich [40]; Heranney [41]; Lantz [43]; Miller [44]; Miller [2];
Radde [45]; Robinson [46]; Tavasoli [52] and high Broberg [38].
Incomplete outcome data (attrition bias)
We found that incomplete outcome data(attrition bias) Abdul
[37]; Abdullah [48]; Broberg [38]; Buehler [39]; de Jonge [50];
Heranney [41]; Jibaja-Weiss [42]; Lantz [43]; Lima [51]; Miller
[44]; Radde [45]; Robinson [46]; Tavasoli [52]; Torres-Mejia [47]
were low risk of bias, Dietrich [40]; Miller [2] were unclear and
Beach [49] was high.
Selective reporting (reporting bias)
Critical appraisal revealed that Abdul [37]; Broberg [38];
Buehler [39]; de Jonge [50]; Dietrich [40]; Heranney [41]; Jibaja-
Weiss [42]; Lima [51]; Radde [45]; Tavasoli [52] were low risk of
bias. Therefore Lantz [43]; Miller [44]; Miller [2]; Robinson [46];
Torres-Mejia [47] were unclear and Abdullah [48]; Beach [49]
were high risk of bias
Other potential sources of bias
We judged as low risk of bias Abdul [37]; Abdullah [48];
Buehler [39]; de Jonge [50]; Dietrich [40]; Jibaja-Weiss [42]; Lantz
[43]; Lima [51]; Miller [44]; Miller [2]; Radde [45]; Robinson [46];
Tavasoli [52]; Torres-Mejia [47] as unclear Beach [49]and Broberg
[38]; Heranney [41] were judged as high risk of bias (Figure 2 & 3).
Summary of Main Results
Call reminders and cervical cancer screening
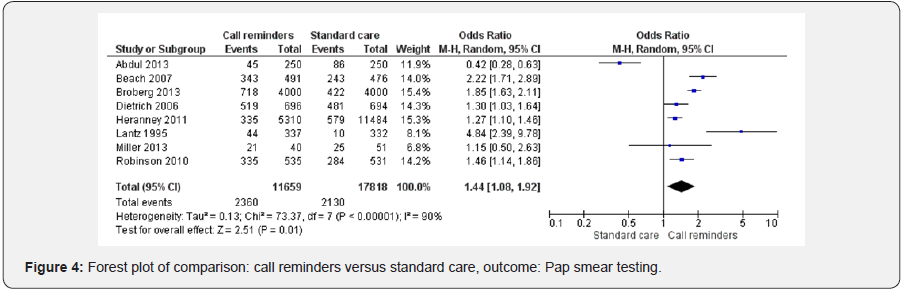
Height studies [2,37,38,40,41,43,46,49] were included in
the forest plot analyzing the effect of call reminders on cervical
cancer screening in risk women. Call reminders were statistically
significant in increasing cervical cancer screening compared to
the standard care (OR 1.44 95% CI 1.08, 1.92, 29477 participants,
8 studies, Heterogeneity: Tau² = 0.13; Chi² = 73.37, df = 7 (P <
0.00001); I² = 90%, random effects). Test for overall effect: Z =
2.51 (P = 0.01) (Figure 4).
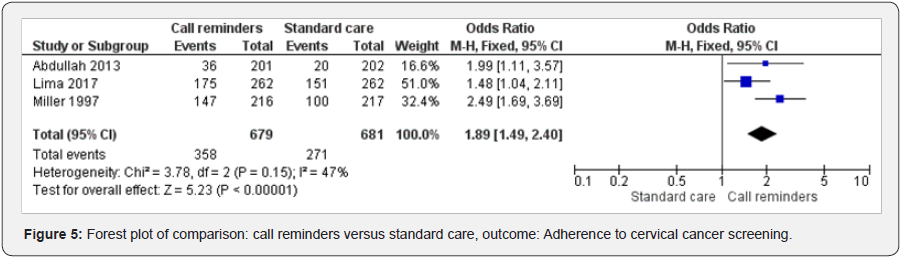
Call reminders and adherence to cervical cancer screening
Three studies [48,51,44] were included in examining the
effect of call reminders on cervical cancer screening adherence.
Call reminders versus standard care has shown statistically
significant results (OR 1.89 95% CI 1.49, 2.40, 1360 participants,
3 studies). Heterogeneity: Chi² = 3.78, df = 2 (P = 0.15); I² = 47%,
fixed effects). Test for overall effect: Z = 5.23 (P < 0.00001) (Figure 5).
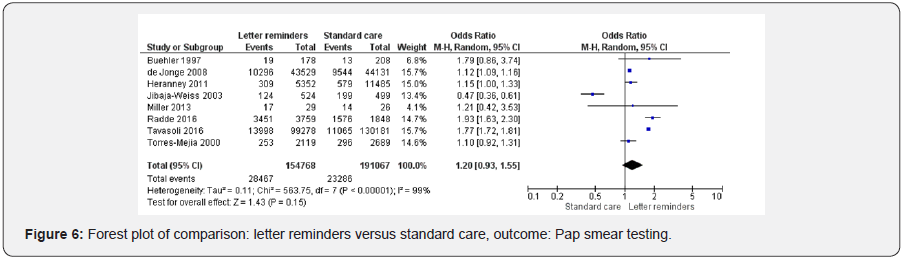
Letter reminders and cervical cancer screening
Height studies were included in letters reminders versus
standard care [39,41,42,2,45,52,47,50]. Letter reminders did not
improve cervical cancer screening (OR 1.20 95% CI 0.93, 1.55,
345835 participants, 8 studies, Heterogeneity: Tau² = 0.11; Chi²
= 563.75, df = 7 (P < 0.00001); I² = 99%, random effects). Test for
overall effect: Z = 1.43 (P = 0.15) (Figure 6).
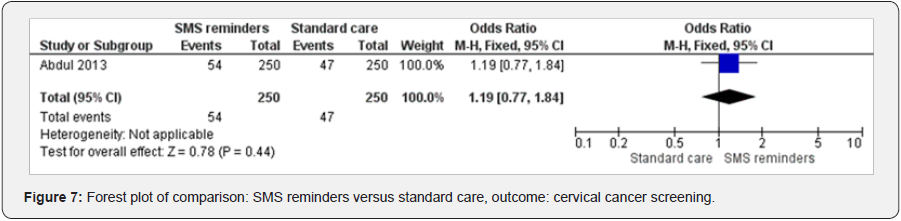
SMS reminders and cervical cancer screening
One study analyzed the effect of SMS reminders on cervical
cancer [37]. SMS reminders increased cervical cancer screening
(OR 1.19 95%CI 0.77 to 1.84, 500 participants, 1 study, test for
heterogeneity not applicable, fixed effects) (Figure 7).
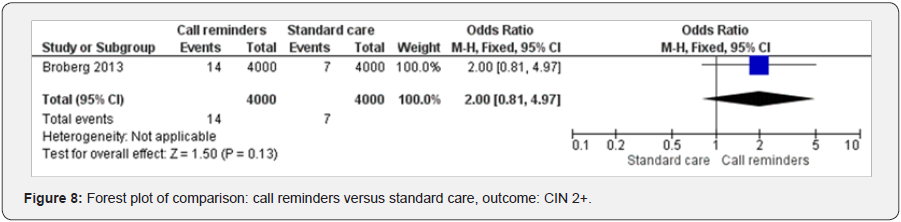
Call reminders and CN 2+
One study examined the effect of call reminders on diagnosing
CN 2+ [38]. The result has shown the call reminders improved CN
2+ diagnostic (OR 2.00 95% CI 0.81 to 4.97, 8000 participants, 1
study, test for heterogeneity not applicable, fixed effects) (Figure 8).
Discussion
The overall completeness and applicability of evidence could
be judged high when we considered the impact of call reminders
on cervical cancer screening and adherence to screening. This
illustrated the strength of this review. Then, this study could
influence public health policy in screening cervical cancer in risk
population. This evidence is strengthened by a recent review
that has shown automated telephone communication systems
interventions can modify patients’ health behaviors, improve
clinical outcomes and increase healthcare uptake with positive
effects in multiple health areas among which immunization,
screening, appointment attendance, and adherence to medications
or tests [63].
Letter reminders have shown to improve cervical cancer
screening outcomes; therefore the results were not statistically
significant compared to recent studies conducted in this field
[45,52]. The quality of evidence was moderate when analyzing
the effect of letter reminders on cervical cancer screening
in risk population. Letter reminders could still constitute an
option in improving cervical cancer screening. However, these
strategies would be challenging to implement in the context of a
jurisdictionally centralized screening program [52].
We found only one RCT that investigated the effect of SMS
on cervical cancer screening. The result was not significant. In
addition, the quality of evidence was moderate. Further studies
should be conducted in this field even if several reviews have
shown positive effect of short messaging on health outcomes.
Only one RCT was found in analyzing the impact of mHealth on the
diagnosis of cervical intraepithelial neoplasia grade 2. The quality
of evidence was moderate; the overall result was not significant.
Therefore, further studies are needful in this field.
Telephone interventions is a resource associated with the
nursing practice, which can produce significant changes in the
health outcomes, highlighting the importance of technical and
clinical knowledge for the interventions by the professional [51].
Furthermore, the use of technology for healthcare development
requires trained professionals to promote the convergence
between human development and technological knowledge,
aiming at the desired goals [51].
The lack of high-quality evidence on the prevention of cervical
cancer for high risk women, which is important for implementing
efficient screening and treatment strategies, results then in the
absence of a clearly defined health program in low and middle
income countries [13]. This is responsible for the low screening
uptake and high mortality rates [13].
As said above, several knowledge gaps might inhibit women
from undergoing cervical cancer screening. This review could
be useful in overcoming certain gaps, and then cervical cancer
screening could be ameliorated.
Authors’ conclusion
Nowadays, the risk of developing cervical precancerous
and cancerous lesions is high; therefore close monitoring and
specific schedule for follow constitute a big challenge. This review
supports the use of call reminders in improving cervical cancer
screening and adherence to testing. The level of evidence is high.Then, call reminders could be suggested to be incorporated
in different national policy in screening cervical cancer in risk
populations. The lack of sufficient evidence on the subject limits
the reliability of the current cervical cancer screening guidelines
for high risk women is the leading cause of diagnosing cervical
cancer in the last stage. Further studies in this field will provide
more solid foundations for preventing cervical cancer. However,
this review could orientate public health policy makers.
Acknowledgment
We are grateful for all the review team in their different contributions.
To know more about Open Access International
Journal of Pulmonary & Respiratory Sciences please click on: https://juniperpublishers.com/ijoprs/index.php
To know more about Open access Journals
Publishers please click on : Juniper Publishers
To know more about juniper publishers: https://juniperpublishers.business.site/

Comments
Post a Comment