Impact of Acute Kidney Injury on the Survival of Subjects Receiving Noninvasive Ventilation-Juniper publishers
JUNIPER PUBLISHERS-OPEN
ACCESS INTERNATIONAL JOURNAL OF PULMONARY & RESPIRATORY SCIENCES
Abstract
Objective: the main objective was to determine
the presence of acute kidney injury (AKI) and the 90-day survival of
subjects with acute respiratory failure (ARF) receiving noninvasive
ventilation (NIV) in the Emergency Department (ED)
Method: We performed a prospective
observational study. AKI was defined as the growth of level of creatinin
between the one made in the ED, which had to be 1.5 times higher than
the "basal value” (within the previous 3 months). Subjects were
contacted by telephone at hospital discharge and at 30, 60 and 90 days
after the initiation of NIV.
Result: We analyzed 174 cases:
30(17.3%)subjects with AKI and 144(82.7%)subjects no-AKI. Fifty-three
percent of the subjects (16 subjects)with AKI died versus twenty percent
(30 subjects)with no-AKI (RR 3.276; CI 95%: 1.74-6.16. P<.001) Cox
regression analysis showed the following to be statistically
significant: subjects with AKI (HR 2.808; CI95%: 1.497-5.291. P=.001),
mean blood pressure (HR 0.969; CI95%:
0. 926-0.994. P=.044)and age (HR 1.039; CI 95%: 1.007-1.71. P=.015).
Conclusion: The presence of AKI is an independent factor of mortality in subjects with ARF requiring NIV in the ED.
Abbreviations:
ARF: Acute Respiratory Failure; ED: Emergency Department; IMV: Invasive
Mechanical Ventilation; NIV: Non Invasive Ventilation; COPD: Chronic
Obstructive Pulmonary Disease; APE: Acute Pulmonary Edema; AKI: kidney
Injury; AKIN: Acute Kidney Injury Network; IPAP: Inspiratory Positive
Airway Pressure
Introduction
The management of acute respiratory failure (ARF)in
the Emergency Department (ED)is evolving from classical invasive
mechanical ventilation (IMV)with endotracheal intubation to the "more
recent” noninvasive ventilation (NIV)[1].
From almost the beginning of the implementation of the latter technique
EDs were considered as fundamental strategic areas since early
initiation of NIV reduces patient mortality [2].
Exacerbations of chronic obstructive pulmonary disease (COPD)and acute
pulmonary edema (APE)are the two most frequent diseases in the ED [1].
Factors associated with failure of NIV and lower patient survival
include a low level of consciousness, high respiratory rate, pH values
less than 7.25, high scores in severity scales(APACHE, SOFA)or
hemodynamic instability [2,3-7]. On adding IMV to these prognostic, it is observable a worsening in the kidney function, which leads to a higher mortality [8-10]. The evaluation of renal function consolidates acute kidney injury (AKI)which is based on the RIFLE [11] and Acute Kidney Injury Network (AKIN)criteria [12].
These criteria present two fundamental points: the first is a dynamic
study of renal function according to changes over time, and the second
is a grading of AKI depending on the relative decline in renal function.
Both scales adequately determine the prognosis of the patient [14-17].
However, studies on factors associated with NIV do not evaluate in
depth the relationship between the renal function and the survival of
these subjects [2-5,14].
Therefore, the aim of the present study is to determine the survival of
subjects receiving NIV and the presence of AKI in the ED.
Methods we performed a prospective observational
study carried out in the ED of the Hospital General Universitario Reina
Sofia of Murcia (Spain)which attends a population of 202,000
inhabitants, with 92,297 emergencies having been attended in 2014. The
study began on November 10, 2012 and finished on June 28, 2014. Patient
recruitment was dynamic and consecutively included all the subjects
attended in the ED. The inclusion criteria for these subjects were:
a. Aged above 18 years.
b. ARF defined by pO2/FiO2<300.
c. NIV during the ED visit.
d. A diagnosis in ED that were of APE or COPD
exacerbation.
The diagnosis for APE was base on clinical's
foundings made by the ED's physician with a chest radiography compatible
with APE. The COPD exacerbation is defined as a worsening of the
patient's respiratory symptoms that is beyond normal day-to- day
variations in subjects with known COPD.
A patient with a serum creatinine value carried out
in the last 3 months. The exclusion criteria were: requirement for a
lifesaving or emergency intervention, the necessity IMV before beginning
with NIV and subjects receiving hemodialysis. The study followed the
prevailing laws and regulation and was approved by the Ethical Committee
of Clinical Investigation of our hospital. All the participants of the
study provided informed consent. Confidentiality of all personal data
was managed according to the Spanish Organic Law 15/1999, of 13 December
on the protection of personal data. The main objective of the study was
to determine the mortality at 90 days after the initiation of NIV and
the presence of AKI. We determined serum creatinine (mg/dl) levels at
admission to the ED. To define the "basal value" we had to use the last
measurement of serum creatinine made to the patient. This measurement
had a deadline of three months. AKI was defined as the growth of level
of creatinine between the one made in the ED, which had to be 1.5 times
higher than the "basal value". The subjects that were discharged were
telephoned at 30, 60 and 90 days after the initiation of NIV. The study
included secondary objectives were the mortality rate during
hospitalization, admission to the intensive care unit (ICU), mortality
at 30 and 60 after the initiation of NIV and mortality according
diagnosis(APE, COPD exacerbation). Mortality was also taken into
account according to the AKIN criteria [13].
NIV was the administration of continuos positive airway pressure (CPAP)
or Bilevel positive airway pressure (BiPAP) applied through a
interface. All subjects were continuously monitored. The ventilators
used for NIV were either BiPAP model ST or Trilogy 202 (Respironics;
Murrysville, PA). The initial ventilator.
Settings are as follows:
I. BiPAP Mode: Inspiratory Positive Airway Pressure (IPAP) between 10-16cm H2O and an Expiratory Positive Airway Pressure (EPAP) of 4cm H2O. After, the pressure (increasing the pressure support in 2 cm H2O each time) was adjusted to achieve an expiratory mean tidal volume of at least 5 ml/kg.
II. CPAP Mode: EPAP of 5cm H2O, increasing the pressure to 10-15 cm H2O.
The IBM SPSS Statistics v-21 was used for the statistical analyses.
Categorical variables were expressed as absolute values and percentages.
Continuous values were expressed as mean, standard deviation and
median. In addition, the type of distribution was determined using the
Kolmogorov- Smirnov test. Differences between categorical variables were
evaluated using the Chi square and continuous variables were analyzed
with the Student's T test if the distribution was normal or the
Mann-Whitney U test if otherwise. The relative risks were calculated
with their 95% confidence intervals (CI 95%). To determine associations
between the continuous variables and the different groups the ANOVA or
Kruskall-Wallis test was used. To discriminate the confounding power of
the variables, Cox regression analysis was used performing univariate
analysis of the statistically significant variables (not only regarding
AKI, but also the mortality) and including the subjects with AKI.
Kaplan- Meier analysis was performed for survival analysis, and the
curves were compared using the Log rank test. A p value < 0.05 was
considered significant.
Results

ARF: Acute Respiratory Failure.
NIV: Noninvasive Ventilation.
COPD: Chronic Obstructive Pulmonary Disease.
APE: Acute Pulmonary Edema.
AKI: Acute Kidney Injury.
A total of 291 cases were included, 52(17.8%) of
which were excluded for lacking serum creatinine determinations in the
previous 3 months, 61(20.9%) presented a different diagnosis
exacerbation of COPD or APE, in 2(0.68%) cases data were lacking and
2(0.68%) were less than 18 years of age. Thus, 174 cases (59.7% of the
subjects) were finally analyzed (Figure 1).
One hundred forty-four subjects (82.7%) didn't have Acute Kidney Injury
(no-AKI), while 30 subjects (17.2%) developed an Acute Kidney Injury
(AKI).Table 1
shows the basal characteristics of the subjects comparing those with
AKI with subjects with no-AKI. Of the 174 subjects studied, 45(25.9%)
died within 90 days of ED discharge. Among subjects with AKI the
mortality at 90 days was 53.3% (16 subjects) compared to 20.1% (29
subjects) in those with no-AKI (RR 3.276; CI 95%:1.74- 6.16.P<.001).
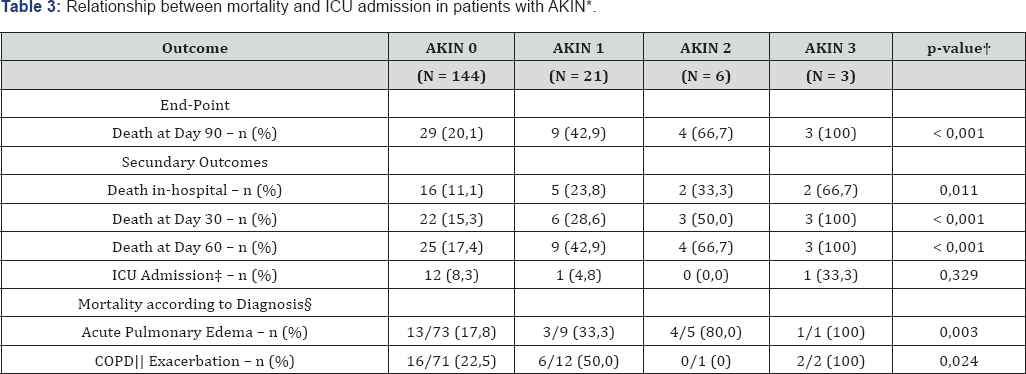
The global in-hospital mortality was 14.3% (25 subjects), 30.0% with AKI
vs 11.1% no-AKI (RR 2.554; CI 95%:1.32-4.92.P=0,007). Tables 2 & 3
show the data related to mortality. Urea, serum creatinine, creatinine
clearance and previous serum creatinine values showed no statistically
significant relationship with 90-day mortality, with P values of .133,
.269, 0118 and .527, respectively. However, the difference in serum
creatinine levels (1.14±0.89 vs. 0.28±0.51 mg/dl; P=.024) were found to
be related to mortality at 90 days. Regarding the in-hospital mortality,
a significative statiscal difference was found as regards the serum
creatinine (1.76±0.93 vs. 1.37±0.68 mg/dl; P=0.014) and the difference
in serum creatinine levels (0.57±0.91 vs. 0.21±0.35 mg/dl; P=.039).
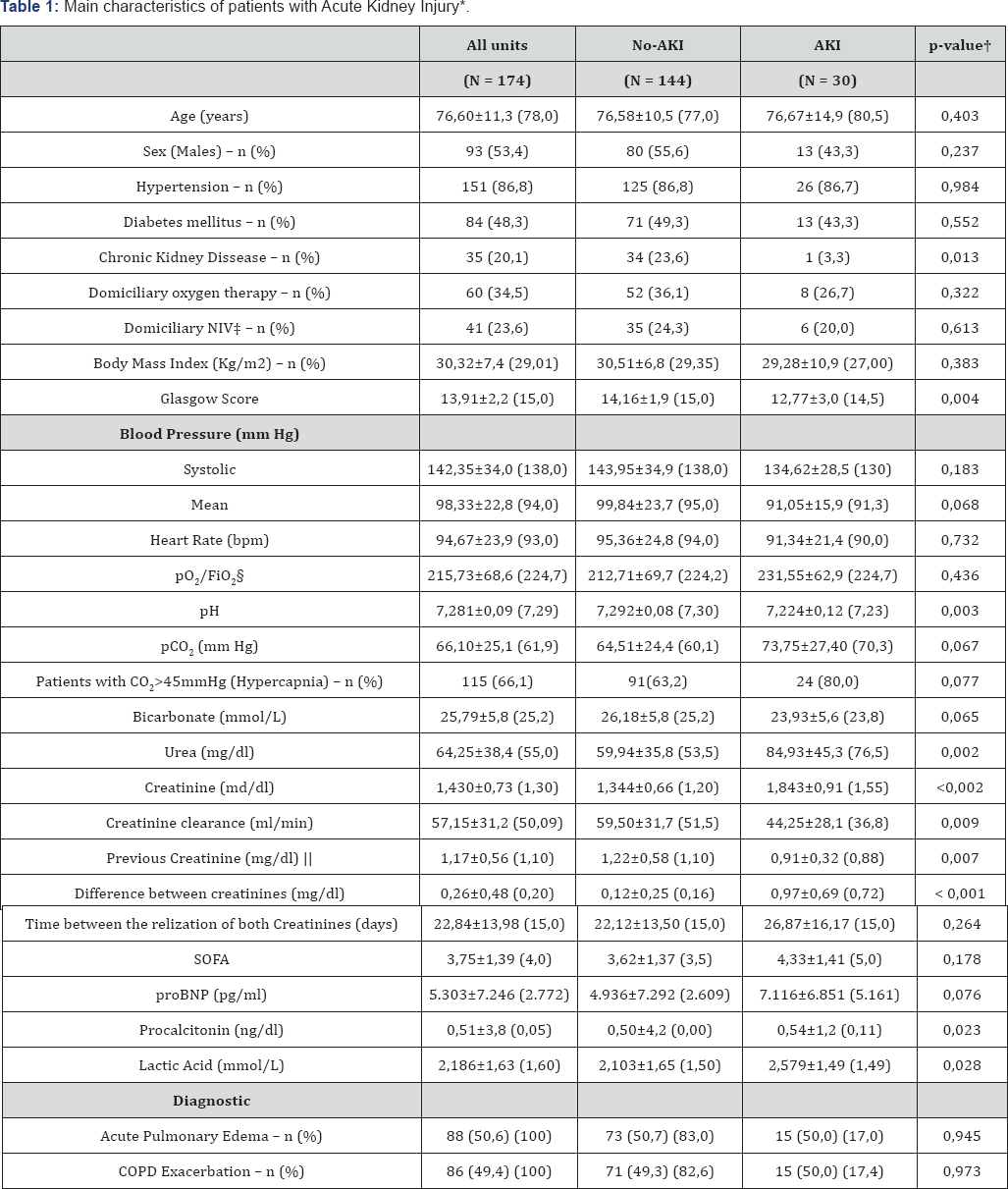
* Continuous values are presented as mean ± SD (median)
† p-value to contrast both groups.
‡ Any type of domiciliary noninvasive ventilator
S Inspiratory oxygen fraction.
‖ Creatinine obtained from analyses in the last three months.
¶In the lowest line the percentage amoung the group are shown.
AKI: Acute Kidney Injury.
NIV: Noninvasive Ventilation.
COPD: Chronic Obstructive Pulmonary Dissease.
SOFA: Sequential Organ Failure Assessment.

* AKI: Acute Kidney Injury.
† p-value to contrast both groups..
‡ ICU: Intensive Care Unit
S The number of event is shown/ total amount within the diagnosis.
‖ COPD: Chronic Obstructive Pulmonary Diseases.
With regard to the remaining variables studied, among
the categorical variables none of them showed a significative statiscal
relationship with 90-day and in-hospital mortality. To the contrary, of
the variables the following were statistically significant: aged
(75.27±11.4 vs 80.40±10.4 years. P=.004), mean blood pressure (100.7±22.
vs 91.3±21.4 mmHg. P=.010), pro BNP (4627.0±6299.5 vs 7244.1±9264.3
pg/ml. P=.040); procalcitonin 0.48±4.4 ng/dl vs 0.59±1.5 ng/dl.
P=.001)and SOFA score (3.5±1.1 vs 4.6±1.7. P=.023) No relationship was
observed between the presence of AKI and the probability of admission to
the intensive care unit (ICUj, with ICU admission of 8.3% in subjects
with no-AKI, in opposition to a 6.7% in subjects with AKI (RR: 0.816; CI
95%: 0.21-3.07; P=.760)(Table 2). The Kaplan-Meier curves (Figure 2)
showed a greater mortality in subjects with AKI on comparing no-AKIN
(P<.001) Cox regression analysis showed statistical significance in
the presence of AKI (HR 2.808; CI 95%: 1.49-5.29; P=.001), mean blood
pressure (HR 0.969; CI 95%: 0.926-0.994; P=.015)and age
(HR 1.039; CI 95%: 1.007-1.071; P=.015) (Table 4).
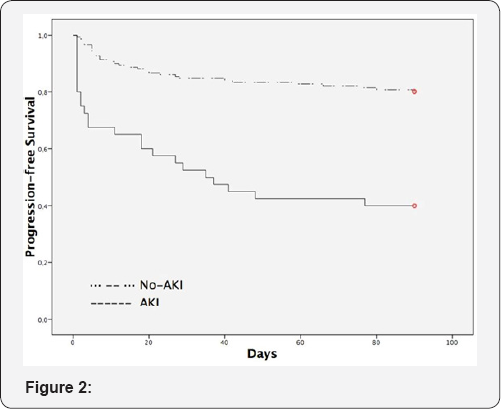
*P < .001. AKI: Acute Kidney Injury.

*HR: Hazard Ratio.
CI: Confidence interval.
AKI: Acute Kidney Injury.
Discussion
This is the first prospective study to evaluate the
association between worsening in renal function and the mortality of
subjects with severe ARF. The severity of both hypoxemic and hypercapnic
ARF is related to the need for NIV. The results of the present study
indicate a lower survival among subjects with worsening in renal
function compared to basal values and the greater the renal failure the
worse the survival. The strength of our study lays in the use of the
initial serum creatinine value compared with a reasonable recent basal
determination. Therefore, the prognostic value of renal function may be
determined at the time of initiating NIV. In the present study we
demonstrate that the presence of renal failure triples the probability
of death. The importance of this study is that it suggests that AKI has a
previously unappreciated relationship among the prognostic factors of
subjects receiving NIV.
The classical study on prognostic factors by Confalonieri et al. [8]
did not include either the presence of renal failure or measurements of
renal function such as serum creatinine or urea. Indeed, serum
bicarbonate values reflecting acid-base equilibrium are often not
included [1,3,7-9].
This study even proposed a prognostic scale including the APACHE. Thus,
a greater mortality is observed with values >29 in the APACHE scale.
In our trial, we have used the SOFA scale in order to predict the
mortality. As it was expected, taking into account the reference
literature, the mortality in subjects with high SOFA was higher
mortality. However, when the multivariate analysis was carried out, the
SOFA scale disappeared from the model because of the presence of AKI. As
the APACHE, SAPS II and SOFA scales included the kidney function, it is
likely that the worsening of the kidney function is an independent
variable and very important in the mortality of subjects undergoing a
NIV. A recent study by Pacilli et al. [3]
reported 18.2% of moderate or severe renal failure in COPD subjects
with hypercapnic ARF requiring NIV. This value is closer to that
observed in our study in which the mean age of the subjects was also
over 75 years.
However, although this study determined the success
of NIV as discharge to a hospital ward from the respiratory ICU, they
observed 28.6% vs. 14.9% of moderate or severe renal failure in subjects
with technique failure. Although only almost statistically significant
(P=.069j, this result is similar to our results. The present study has
the advantage of being prospective and having renal function as its
principal objective. However, on analyzing the relationship between
serum creatinine levels and mortality, again no differences were found,
except for the in-hospital mortality where it could be found. This
corroborates the argument that acute worsening in renal function is a
fundamental factor for prognosis, being stronger than punctual
measurement of renal function [14,18-19].
Therefore, in cases in which basal serum creatinine levels are not
available, the use of serum creatinine can help the emergency physician
to come to a decision. With respect to IMV the study by Nim et al. [19]
reported that subjects with an increase in serum creatinine levels
above 0.3 mg/dl within 24 hours and basal serum creatinine levels ≤1.4
mg/dl carried an in-hospital mortality of 56%. The mortality in the
group without an increase in basal serum creatinine was 36%. Although
the mortality rates in our study were not as high, our results support
the results of this group since the mortality rate tripled in our study
(30% in the group with AKI and 11% in subjects without). The "low"
mortality rate in our study is probably due to its having been performed
in subjects with NIV, because the IMV behaves as independent factor of
mortality in subjects with AKI [10].
This proves that the kidney function is a determinant factor in the
prognosis made to subjects with ARF undergoing mechanical ventilation,
both invasive and non invasive. Our trial wasn't designed to
monitorizated the creatinin's levels after the initiation of NIV. Hence,
the weight of the NIV as factor in the development of AKI is unknown
nowadays. Therefore, more researches are needed. As mentioned
previously, bicarbonate levels are often not included as a prognostic
factor of NIV, but have a low predictive power [5].
However, studies describing a relationship have
observed that high levels of bicarbonate (greater than 25 mmol/L) carry a
better prognosis [3,4].
We did not find a relationship between serum bicarbonate levels and
mortality but we did observe lower levels in the presence of AKI.
Traditionally, the pH has been given a very important factor to
prognosis. Therefore, the lower the pH, the worst the prognosis [6,7]. However, in our trial as well as in others [1],
a relationship between and the prognosis was not observed. Similary,
the same can be said for the pCO2. The classical hypothesis was that a
higher level of pCO2 led to a lower pH and, therefore, a worse prognosis
[7-8].
Moreover, our study as well don't prove this. Hence, there has to be
another important factor that influenciates in the pH as well as in the
prognosis. One explanation for the behave of the pH, pCO2 and HCO3-, may
be that subjects with mainly hypercapnic ARF require an increase in
serum bicarbonate to compensate for the associated acidosis. If these
subjects presented AKI they would not be able to increase bicarbonate
levels and consequently their pH levels would be lower. Since AKI
carries a higher mortality this would explain the association between
the higher mortality, low pH levels and not high serum bicarbonate
levels as described in previous studies [1-6].
The main limitation of the present study is the
different use of the AKIN criteria. These criteria are based on changes
in serum creatinine or diuresis once the patient has been admitted.
However, we evaluated the changes between serum creatinine levels at
admission and within the previous 3 months. These "recent" serum
creatinine levels were chosen with the aim of detecting subjects with
AKI earlier since strict use of the AKIN criteria leads to a delay
during which these time-dependent pathologies may worsen. The second
limitation of the study is the cutoff of 3 months for creatinine levels.
This time point was selected with the aim of having relatively "recent"
values to carry out the study. Notwithstanding, in almost 20% of the
cases the previous serum creatinine levels were not available. The last
limitation is the relative small number of subjects with AKI. This fact
is made worse in subjects classificated as AKIN 2 and AKIN 3. Therefore,
it is fundamental for the research of more studies that valorate the
behave in the changes in the kidney function in subjects undergoing NIV.
Strangely enough subjects with AKI do not possess a higher possibility
of being in ICU admission. Once more, the kidney function is the
forgotten one in subjects undergoing a NIV. This study is just the first
step. It is clear that the way we deal with AKI subjects has to change.
The best path is yet to be discovered. In conclusion, the presence of
AKI measured according to the AKIN criteria is an independent factor of
mortality in subjects with ARF requiring NIV in the ED.
To know more about Open Access International
Journal of Pulmonary & Respiratory Sciences please click on: https://juniperpublishers.com/ijoprs/index.php
To know more about Open access Journals
Publishers please click on : Juniper Publishers
To know more about juniper publishers: https://juniperpublishers.business.site/


Comments
Post a Comment