A Case of Mycobacterium Simiae Mimicking Malignancy-Juniper publishers
JUNIPER PUBLISHERS-OPEN
ACCESS INTERNATIONAL JOURNAL OF PULMONARY & RESPIRATORY SCIENCES
Introduction
In 1965, Mycobacterium simiae was first isolated from macaques [1]. Isolation of M. simiae has been mostly confined to the Southern US, Israel, and Cuba but is increasingly reported worldwide [2-3]. In the University Hospital in San Antonio, Texas, M. simiae has become the second most frequently isolated non- tuberculous mycobacterium surpassed only by Mycobacterium avium
complex. Out of patients analyzed in this facility during an 11 year
period, 10% had definite infection and 76% were thought to be colonized [4]. M. simiae
often colonizes the airway, but clinical disease has been increasingly
reported especially in immunocompromised patients and those with an
underlying lung disease.
Case Report
A 56-year-old woman with a prior history of breast
cancer presented to clinic with a productive cough, malaise, hoarseness
and myalgia. She denied night sweats, weight loss, wheezing, or
hemoptysis and indicated that all symptoms resolved on their own except
for the productive cough. The patient has a history of invasive
carcinoma of the right breast (diagnosed in 2008). A CT scan reported
scarring at bilateral apices and lingual as well as tree-in-bud-
opacities in the right middle lobe. A transthoracic biopsy of the right
middle lung performed prior to chemotherapy initiation showed active
granulomatous inflammation and scattered epithelial cells of uncertain
significance. A PET- CT, showed moderately increased pathologic activity
that corresponded to a pleural based soft tissue structure in the area
of the right middle lobe. Sputum cultures where negative and the patient
proceeded with treatment with adjuvant radiation, bilateral mastectomy
and hormonal therapy.
In 2014 the patient had a positive acid-fast bacilli
(AFB) sputum sample and was referred to an ID specialist. She was
prescribed antibiotics that included clarithromycin and ethambutol
however, due to severe reflux the therapy was aborted. Upon a follow up a
chest x ray a nodular opacity at the right lung was observed. A CT scan
revealed bronchiectasis in the right upper lobe and lingula, as well as
characterized the pulmonary nodule as a measuring 12 x 10 sub-solid
nodule. Sputum samples were sent for AFB and fungal cultures, no growth
was reported. The patient had a bronchoscopy performed, with
transbronchial biopsies showing no evidence of malignancy or granuloma. A
bronchoalveolar lavage was positive for M. simiae, no treatment
was initiated at that time. Follow up CT scans where performed every 3
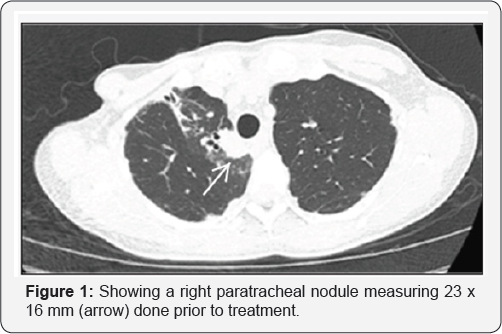
to 6 months. A new solid, spiculated masslike lesion measuring 22 x 17mm
and adjacent to the trachea was seen in the right upper lobe. This
lesion was not observed on a CT scan performed 4 months before. A PET CT
showed a high avidity of this nodule, with an SUV of 10.3 at the right
upper lobe nodule (Figure 1 & 2).
Given the location of the nodule adjacent to the
trachea and concern that this could be recurrent breast cancer, an EBUS
was performed. Results revealed granulomatous inflammation with a
positive AFB stain on FNA samples. BAL cultures obtained from the right
upper lobe grew M. simiae. The patient was initiated on TMP/SMX
(800/160mg), azithromycin (500mg), and ethambutol (800mg) each taken
once daily. Levofloxacin was not used due to a reported allergy to
quinolones. The patient was evaluated 3 months later with improved
symptoms. On CT scan, the right upper lobe lesion had decreased in size
and the area of tree-in-bud infiltrate had improved.

The uniqueness of this case is the presentation of M. simiae infection and its development into a hypermetabolic nodule with rapid growth. An early report by Bell and coworkers found M. Simiae was a frequent colonizer of sputum but rarely cause disease [5].
However, a more recent report from our institution, suggested that the
organism was pathogenic in up to 20% of patients if both definite and
probable diagnosis were considered. In study between 1999-2006 from the
Netherlands, Van Ingen et al. [6] described M. simiae
isolated from patients with abnormal chest radiographs. Only 11%
presented as suspected malignant lesions on chest radiography. Data from
this cohort show that M. simiae isolates where cultured mostly
from sputum (44%) and bronchoalveolar lavage (52%) samples. However,
lung biopsy specimens reported growth in only 4% of the samples. It is
difficult to determine the actual percent of patients with M. simiae
disease in this study. However, the American Thoracic Society
Guidelines state that in any patient with systemic symptoms, an abnormal
chest radiograph, and a positive culture of a nontuberculous
mycobacteria (NTM) from BAL fluid could be considered to have active
disease [7].
Yet, it is unclear if this standard should be applied to NTM organisms
with low pathogenicity. In our case, the FNA performed by EBUS showed
granulomatous inflammation and was AFB positive from the patient's
pulmonary nodule. However, M. simiae was only grown from the BAL
culture. The patient responded well to NTM therapy with resolution of
infiltrate and reduction in the size of her pulmonary nodule. This case
points out the difficulty of diagnosing M. simiae disease and the diagnostic utility of performing EBUS to obtain additional tissue from pulmonary nodules or lymph nodes.
To know more about Open Access International
Journal of Pulmonary & Respiratory Sciences please click on: https://juniperpublishers.com/ijoprs/index.php
To know more about Open access Journals
Publishers please click on : Juniper Publishers
To know more about juniper publishers: https://juniperpublishers.business.site/

Comments
Post a Comment