The Value of Positron Emission Tomography in the Mediastinal Lymph Node Metastasis of the Patients Operated for Non-Small Cell Lung Cancer-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS INTERNATIONAL JOURNAL OF PULMONARY & RESPIRATORY SCIENCES
Abstract
Background: In recent years, Positron Emission
Tomography (PET-CT) has been used increasingly in the diagnosis of
thoracic malignancies, in the evaluation of staging, distant organ
metastasis, and post-chemotherapy response. The role of PET/CT in the
mediastinal lymph node stage still remains controversial due to its high
false positives and false negatives.
Aim: We aim to evaluate the diagnostic value
and false negative and positive results of PET/CT on the mediastinal
lymph node metastasis in the patients operated for Non-Small Cell Lung
Cancer (NSCLC).
Material and Methods: The study included 164
patients with NSCLC who underwent mediastinoscopy or anatomic resection
with mediastinal lymph node dissection between January 2008 and January
2018 in Trakya University Thoracic Surgery Department. There were 34
females, 130 male patients whose ages were between 20-88 years (mean:
60,5). We retrospectively compared the mediastinal lymph node
involvement preoperatively PET-CT findings and histopathologic results
in patients with NSCLC who were not received previously chemotherapy or
radiotherapy. Metabolic characterizations of mediastinal lymph nodes and
SUVmax values were recorded.
Results: A total of 682 lymph node samples
were performed in this study. The median five lymph nodes (4-13 lymph
nodes) dissection was performed per average case. The mean SUVmax value
of the True Negative, True Positive, False Negative and False Positive
cases was 0,29(0-1,8); 2,96(1,8-6,4); 0(0); 3,4(1,9-6,8), respectively.
Also sensitivity, specificity, positive predictive value, and negative
predictive value for mediastinal lymph nodes were found 77,7%, 93,5%,
38,8% and 92,9%, respectively.
Conclusion: We conclude that, invasive
mediastinal staging with video mediastinoscopy (VAM) should be performed
in NSCLC due to low sensitivity and positive predictive value of PET
CT.
Keywords: Thoracic Surgery; PET/CT; Lymph node; Non-Small Cell Lung Tumor
Abbreviations:
TN: True Negative; TP: True Positive; FN: False Negative; FP: False
Positive; PET-CT: Positron Emission Tomography; CT: Computerized
Tomography; NSCLC: Non-Small Cell Lung Cancer; EBUS: Endobronchial
Ultrasonography
Introduction
In recent years, Positron Emission Tomography
(PET-CT) has been used increasingly in the diagnosis of thoracic
malignancies, in the evaluation of staging, distant organ metastasis,
and postchemotherapy response [1,2].
PET-CT is a new imaging format that provides metabolic and anatomical
information about the tumor. Non-invasive imaging using tomographic
images and quantitative parameters that reflect the perfusion, metabolic
activity and vitality of the tissues [3].
Since PET-CT images have been anatomic localization and spatial
resolution insufficiency, the anatomical localization of the lesions can
be performed frequently and the sections are combined using
Computerized Tomography (CT) and this is called PET-CT. False positivite
lesions are with high 18-fluorodeoxyglucose (F18-FDG) uptake when not
malignant and false negativites are low-F18-FDG uptake lesions when they
are malignant. The role of PET / CT in the mediastinal lymph node stage
still remains controversial due to its high false positives and false
negatives. Invasive staging methods continue to be the gold standard in
the stage of the metastatic lymph node [4].
We aim to evaluate the diagnostic value and false negative-false
positive results of PET/CT on the mediastinal lymph node metastasis in
the patients who underwent mediastinoscopy or anatomic resection for
NonSmall Cell Lung Cancer (NSCLC).
Material and Methods
In this study; we analyzed the mediastinal lymph node
involvement preoperatively PET-CT findings and histopathologic results
in patients with NSCLC who were not received previously chemotherapy or
radiotherapy. NSCLC was diagnosed in all patients by bronchoscopy, fine
needle aspiration biopsy or intraoperative frozen sections. The study
included patients with NSCLC who underwent mediastinoscopy or anatomic
resection with mediastinal lymph node dissection. Patients under 18
years of age, given chemo-radiotherapy chemo-radiotherapy, non-NSCLC's,
uncontrolled diabetics, N1 positive tumors were excluded from the study.
The cases were evaluated according to age, sex, tumor type, Maximum
standart uptake value (SUVmax) values of mediastinal lymph nodes,
pathology and PET/CT imaging results. Oral intake was stopped 6-8 hours
before the shots, and blood glucose level were kept below 150 mg /dl in
all cases. After blood glucose level and blood pressure was measured, 18
F FDG dose (8-15 mCi/kg) calculated according to body weight was
administered intravenously. After injection, the patients were taken to
the waiting room about 45-60 minutes. The PET/CT device (G.E. Discovery
STE8), a combination of a tomography unit with a cross-sectional
thickness of five mm and a PET unit containing a Bismuth Germenate block
detector, was used for the thorax images of the cases. Images were
taken from the upper part of the vertex to the middle of the thigh.
PET/CT results were assessed by nuclear medicine specialists.
We analyzed retrospectively 164 patients who operated
for NSCLC and who had PET-CT imaging between January 2008 and January
2018 in TTakya University Thoracic Surgery Department. Metabolic
characterization of mediastinal lymph nodes and SUVmax values were
recorded. There were 34 females, 130 male patients whose ages were
between 20-88 years (mean: 60,5). For every patient, SUV max values were
calculated and sizes of the lesions and lymph nodes were measured.
Finally, PET-CT results were compared with histopathologic data. It was
aimed to evaluate the involvement of PET-CT in the mediastinal lymph
nodes together with the pathologic outcome, to determine false
negativity and false positives. The mean SUVmax values of mediastinal
lymph nodes were calculated according to pathology results. All tumors
with malignant mediastinal lymph node involvement in PET-CT, especially
central located or over 3 cm in diameter tumors were first performed
VAM. Patients with mediastinal lymph node metastasis detected by VAM
were sent to oncologic treatment. An anatomic resection and a
mediastinal lymph node dissection were performed in the patients who
were not detected with metastasis by VAM or peripherally located
squamous tumors less than 3 cm in diameter without VAM. Complete
thoracic lymphadenectomy was routinely performed; it consisted of enbloc
resection of all lymph nodes that were accessible in the mediastinum
and hilum of lung. Intraoperative N2 was not detected.
Data Analysis
A statistical analysis was performed using the
Statically Package for the Social Science program (SPSS, 20.0)
Demographics, pathological data and PET/CT results are expressed in mean
values. Frequencies and percentages were used for the categorical
measures. Sensitivity, selectivity, positive predictive value, negative
predictive value and accuracy criteria were used for comparison of the
different diagnostic methods.
Results
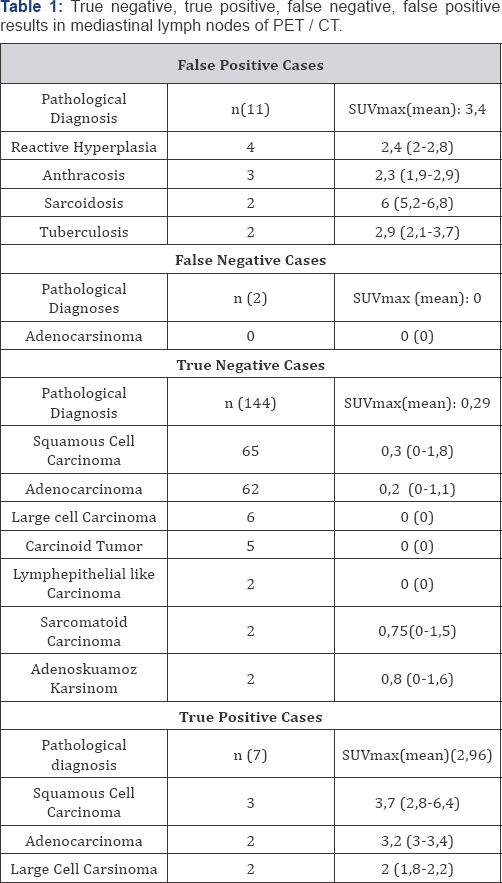
*False positive (FP) = 11 cases SUVmax = 3,4 (1,9-6,8)); False negative (FN) = 2 cases SUVmax 0
*True Positive (TP) = 7 cases SUVmax = 2,96 (1,8-6,4); True negative (TN) = 144 cases SUVmax 0,29 (0-1,8)
SUVmax: Maximum Standardized Uptake Value
In 146 cases mediastinal lymph node involvement was
not detected, whereas in 18 cases, mediastinal lymph node involvement
was detected in favor of malignancy in PET/CT. Four ofthis 18 case first
performed the endobronchial ultrasonography (EBUS) fine needle biopsy,
but none were diagnosed. VAM was performed 72 patients included these
also 18 patients. True positive was 7 patients: Four patients (upper
paratracheal n:2, lower paratracheal n:1, subcarinal n:1) with N2
detected in VAM and these patients received chemotherapy. N2 lymph node
positivity was detected in three cases (subcarinal n:2, paraaortic n:1)
after postoperative pathological examination. These cases were sent to
adjuvant chemotherapy. Other 11 of 18 cases was false positive cases,
surgical resection continued in these cases (Table 1).
Subcarinal lymph node was detected tumor positive in
two of 146 PET / CT metastases negative mediastinal lymph node by
mediastinoscopy and thoracotomy and patients recieved chemotherapy (Table 1).
Lymph node negative patients were operated. After the histopathologic
examination, 35 patients(21,3%) were in stage IA, 54(32,9%) patients in
stage IB, 43(26,2%) patients in stage IIA, 23(14%) patients in stage
IIB, 9 (5,4%) patients in stage IIIA. 160 patients underwent surgery.
Lobectomy for 114 (22 of them was VATS lobectomy), pneumonectomy for 27,
bilobectomy for 11, and segmentectomy for 8(2 of them was VATS
segmentectomy) were performed. Tumor histopathological types were
squamous cell carcinoma in 73 patients, adenocarcinoma in 68 patients,
other 19(large cell n:8, 5 carcinoid n:5, lymphoepithelioma-like
carcinoma n:2, sarcomatoid type lung carcinoma n:2, adenosquamous
carcinoma n:2). Median SUVmax values of malignant / benign tumors of
mediastinal lymph nodes can be seen in Figure 1.

PET/CT: Positron Emission Tomography / Computed
Tomography; TN: True Negative; TP: True Positive; FN: False Negative;
FP: False Positive
A total of 682 lymph node samples were removed in
this study. The median five lymph nodes (4-13 lymph nodes) dissection
was performed per average case. True Negative (TN), True Positive (TP),
False Negative (FN), False Positive (FP)results in mediastinal lymph
nodes of PET / CT was summarized in Table 1.
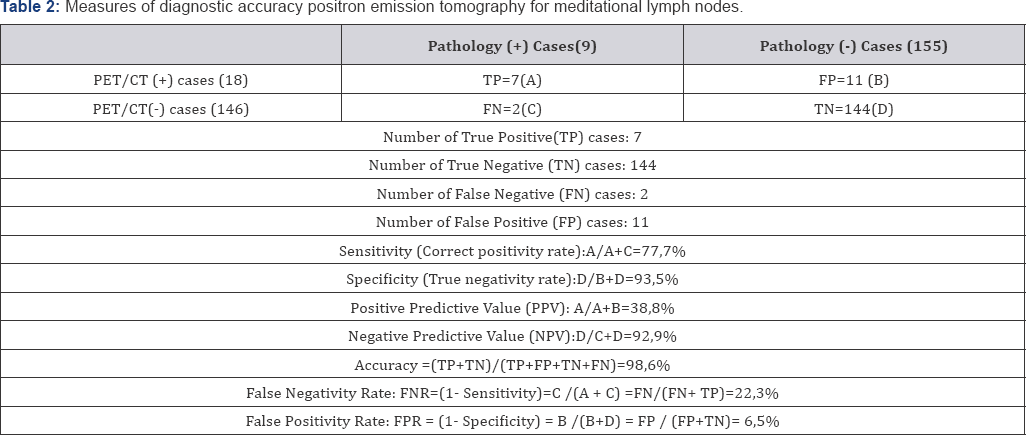
The mean SUVmax value of the TN, TP, FN and FP cases were 0,29 (0-1,8);
2,96 (1,8-6,4); 0(0); 3,4 (1,9-6,8), respectively. The TP lymph nodes
were greater than 1 cm in diameter and two patients'with FN of lymph
nodes was smaller than 1 cm in diameter. Sensitivity, specificity,
positive predictive value, and negative predictive value for mediastinal
lymph nodes were found 77,7%, 93,5%, 38,8% and 92,9%, respectively (Table 2).
Discussion
PET/CT has been widely used in the diagnosis of
thoracic malignancies, staging, determination of distant organ
metastasis and evaluation of post-chemotherapy response. Treatment
protocol is closely related to the stage of the disease in patients with
NSCLC. For this reason, proper staging is great importance in NSCLC.
The rate of mediastinal lymph node involvement at diagnosis is 28%-38%.
However PET/CT as a new imaging method in diagnosis and staging of lung
cancer, many studies have reported false positives and false negatives
of it. Also PET/ CT has a low sensitivity and positive predictive value
(PPV). This can lead to many overdiagnosis or misdiagnosis in daily
practice. Many studies in the literature on PET/CT mediastinal lymph
node evaluation for non-small cell lung tumors has shown that
sensitivity, specificity, positive and negative predictive values are
higher than only CT [1-6].
F18-FDG is not a cancer specific agent; but it also may be positive
uptake sarcoidosis, tuberculosis, fungal infection, and cerebral
abscess. However, unlike benign pathologies, FDG uptake following
malignant lesions is partially beneficial in differential diagnosis [5].
In the study conducted by Bellek et al. [7]
sensitivity, specificity, PPV, NPV and accuracy for staging mediastinal
lymph nodes were 86,7%, 65,5% , 56,5%, 90,5% and 72,7%, respectively.
The false-negative rate was 13,3 % while the false- positive rate was
34,5% according to their study. In our study, sensitivity was 77,7%,
specificity was 93,5%, PPV was 38,8%, NPV was 92,9% and accuracy was
98,6%. Our findings are consistent with previous literature and the PPV
is lower than the NPV. As the reason for this, infectious and
inflammatory diseases is responsible for false positive results.
The literature on false positive or false negative results of PET-CT is limited. Takamochi et al. [8]
reported the false positive rate as 14% and false negative rate as 20%.
False negativity rate was 22,3% and false positivity rate was 6,5% in
our study. All infections and inflammations with active macrophages,
especially granulomatous diseases, are known to be caused by the
potential false positives in PET/CT. The most common causes of false
positives are tuberculosis, sarcoidosis, coccidomycosis, aspergillosis
and some other infections. On the other hand, low metabolic activity
tumors may give false negative results in PET/ CT. In addition, due to
the limited spatial resolution of PET / CT, the false negative result
rate is increased in lesions smaller than 1 cm (especially <6 mm).
Hyperglycemia may also potentially lead to false negativity because
competitively inhibited FDG may reduce tumor "uptake" [5-9].
While PET-CT study was evaluated; false positive and false negative
findings should be considered. Muscle tissue, brown adipose tissue,
various physiological involvements such as thymus hyperplasia after
chemotherapy, lung or mediastinal infections or inflammations, and
non-malignant tumors-related involvement lead to false positive results [9].
In our study, low sensivity and fairly low positive predictive value
was detected. This attributed to 11 cases detected as false positive due
to reactive hyperplasia, anthracosis and granulomatous inflammation.
This is due to the high incidence of infectious diseases in our country.
Also false negative two cases with less than 1cm tumor positive
mediastinal lymphadenopathy. Because the sensitivity of PET/ CT is very
low in lesions smaller than 1 cm [10]. Kandemir et al. [11]
reported that when the SUV(max) value of 2,5 was used, the sensitivity,
PPV, and diagnostic accuracy of the PET/CT were 100%, 65,4%, and 65,4%
respectively. Also they were calculated the SUVmax cut-off value with
the highest diagnostic accuracy (75%) as 6.3. They concluded that
although a SUVmax cut-off value of 6.3 increases specificity and
diagnostic accuracy, the value of 2,5 and above can give more optimal
results.
In the meta-analysis de Langen et al. [12]
reported that the lymph nodes measured smaller than 1cm without FDG
uptake, malignancy was detected in less than 5% of them. Therefore there
was no need for further mediastinal examination in these cases.
According to the European Society of Thoracic Surgeons, in case of
computed tomography enlarged than 1cm or PET/ CT positive mediastinal
lymph nodes, tissue confirmation is indicated. First endobronchial
ultrasonography (EBUS) or esophageal ultrasonography (EUS) should be
tried, if negative mediastinoscopy should be performed. When there are
no enlarged lymph nodes than 1cm in CT and when there is no uptake in
lymph nodes on PET-CT, direct surgical resection with systematic lymph
node dissection is indicated for periferical located and <3 cm
tumours [13].
In our study VAM was performed in cases with lymph node larger than 1cm
and PET/ CT positive. EBUS/EUS was performed only PET/CT positive four
patients but none were diagnosed. When there are no enlarged lymph nodes
than 1cm in short axis on CT and when there is no uptake in lymph nodes
on PET-CT, direct surgical resection with systematic nodal dissection
is performed for tumors <3cm and peripheral except central tumors or
N1 nodes, adenocarcinoma, tumors 3cm> and FDG positive lymph nodes.
Conclusion
We conclude that; evaluation of mediastinal lymph
nodes by PET-CT alone is not appropriate for the stage of non-small cell
lung cancer. The granulomatous-infectional diseases may lead to false
positive results. In the mediastinal lymph node stage of NSCLC, for
PET-CT positive lesions, the choice between endoscopic staging with
EBUS/EUS and transbronchial biopsy or VAM depends on experience to
minimal requirements for staging.
To know more about Open Access International
Journal of Pulmonary & Respiratory Sciences please click on: https://juniperpublishers.com/ijoprs/index.php
To know more about Open access Journals
Publishers please click on : Juniper Publishers


Comments
Post a Comment