Mounier Kuhn Syndrome: A Rare Variety of Bronchial Dilatation-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS INTERNATIONAL JOURNAL OF PULMONARY & RESPIRATORY SCIENCES
Abstract
Background: Mounier Kuhn’s syndrome is a
rare condition. It is characterised by an increase in the diameter of
the trachea and main bronchi. Imaging plays a fundamental role in
confirming the diagnosis. This syndrome is little known and has not
benefit of enough studies allowing a better comprehension of its
pathophysiology and a performing therapeutic approach.
Case presentation:In this paper, we report the
case of a 53-year-old man suffering from recurrent respiratory
infections. Imaging has made the diagnosis of Mounier Kuhn syndrome by
showing an increase in the diameter of the trachea and main bronchi. The
treatment was based on physiotherapy and appropriate antibiotic therapy
in case of infectious outbreak.
Conclusions: This long-neglected “orphan
disease” should receive more research attention in order to provide
better understanding of its aetiology, pathogenesis and multimodality
treatment.
Keywords: Mounier Kuhn Syndrome, Tracheal Dilatation,Bronchial Dilatation, Congenital and Rare Disease, Radiological Diagnosis
Background
Mounier Kuhn’s syndrome is a rare and congenital
disease. It is characterized by an increase in the size of the trachea
and main bronchi caused by a congenital disorder of the connective
tissue and smooth muscles of these structures, the distal bronchial tree
is usually normal. Its diagnosis is accomplished with the
use of Computed Tomography (CT). It can be associated with other
congenital conditions, which makes the understanding of its
physiopathology more complicated. Its clinical features vary from being
asymptomatic to severe respiratory distress. However, therapy remains
conservative [1].
Case Report
Mr AB, a 53 years old non-smoking patient and father
of 7 children, with a history of recurrent respiratory infections. He
was admitted for a cough and purulent sputum evolving in a context of
deterioration of the general state. Clinical examination showed
bilateral ptosis, polypnea at 22 breathes per minute, sonorous bilateral
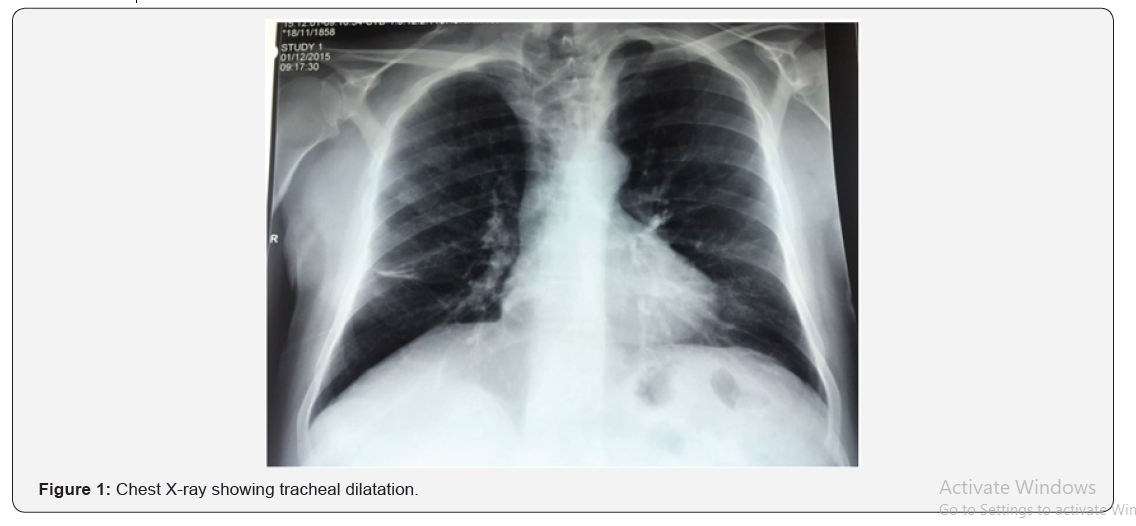
rales in pleuro-pulmonary auscultation and a fever at 38.5 °C. Chest
X-ray showed tracheal dilation (Figure 1).
Blood tests found a CRP at 75mg/l, white blood cells at 12,500/mm3
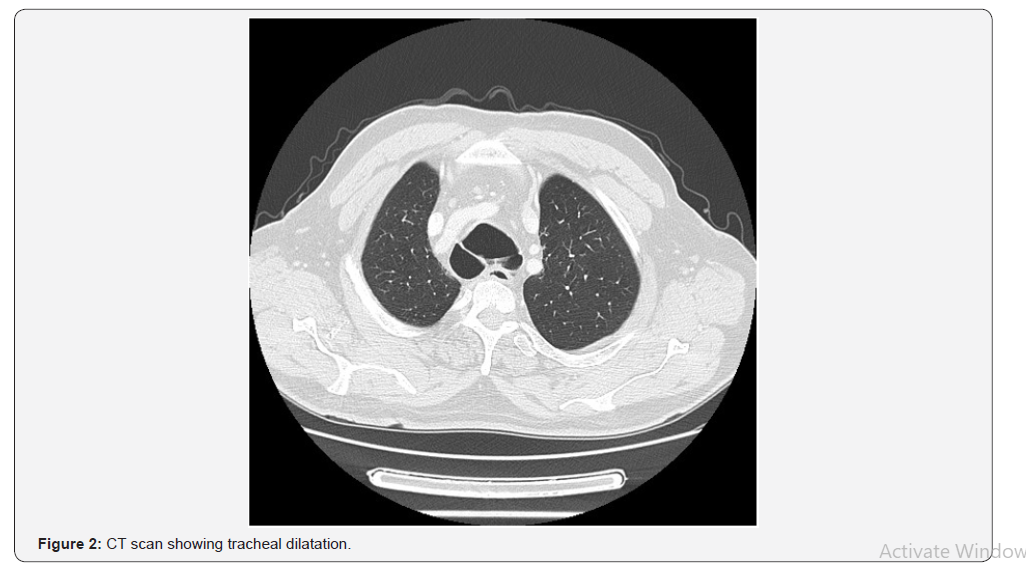
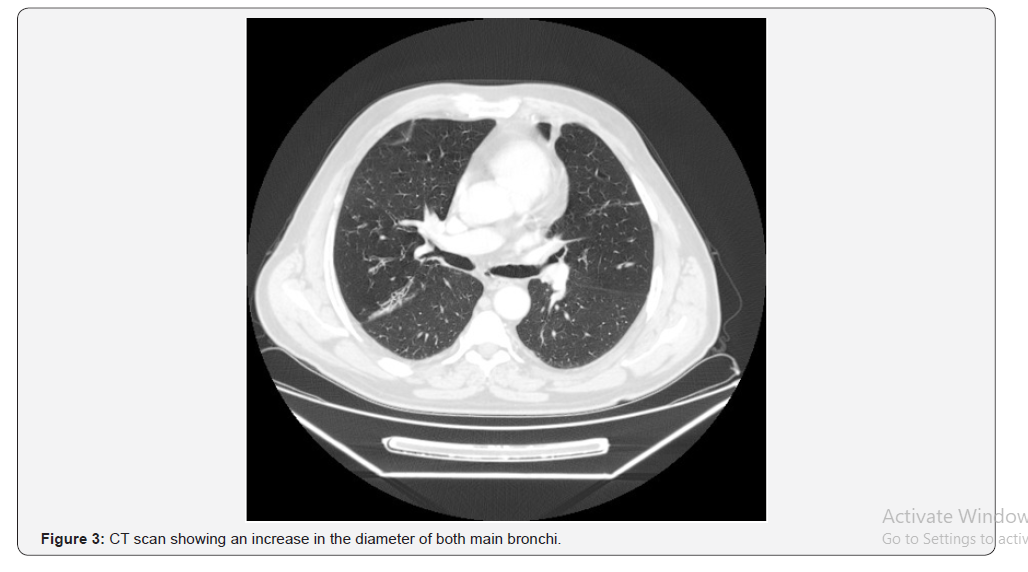
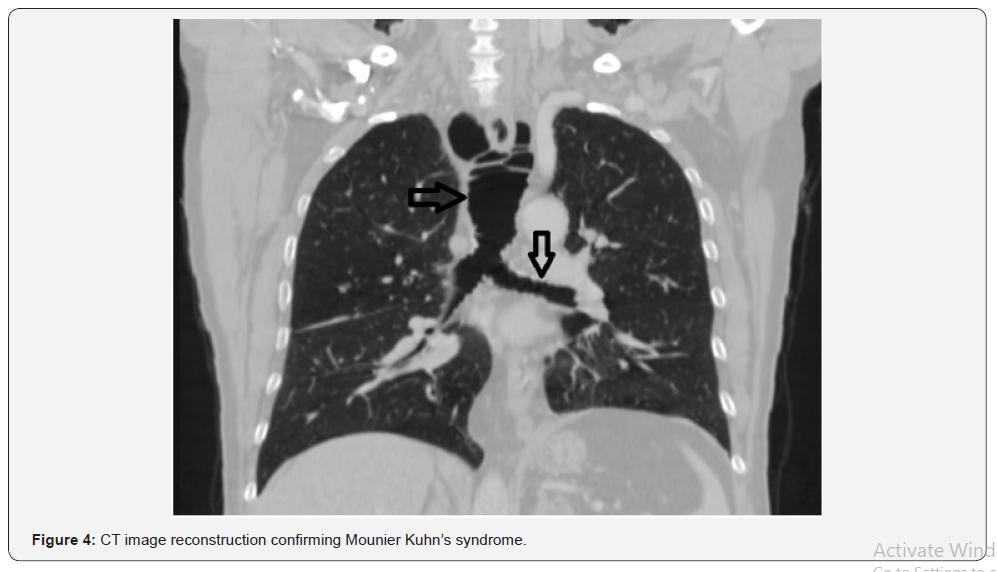
predominantly of neutrophils at full blood count. Thoracic computed
tomography was conducted (Figures 2-4) and revealed tracheal dilation
with a diameter of 35mm (whereas the normal diameter should not exceed
25mm in humans), and dilation of main stem bronchi with a diameter of
25mm on the right and 26mm on the left.
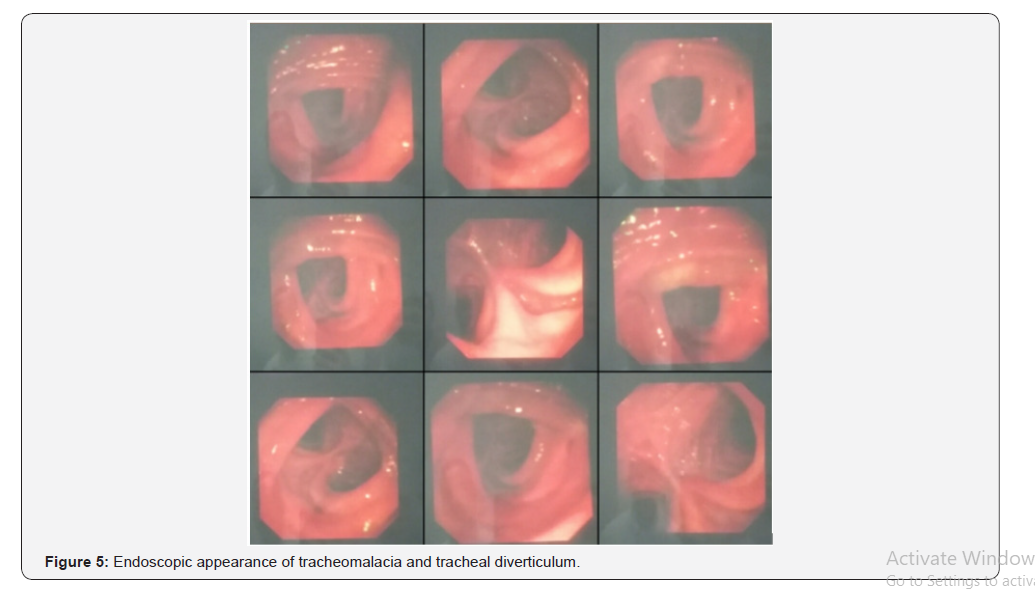
Bronchial fibroscopy demonstrated an inflammatory
aspect of the mucosa with tracheomalacia and tracheal diverticulum
(Figure 5). Spirometry was suggestive of obstructive abnormality with
poor bronchodilator reversibility, Alpha-1 antitrypsin was 255mg/dL
(100-300mg/dL), nasal endoscopy did not reveal any polyposis and the
spermogram was not performed (patient, father of 7 children). The
diagnosis of a Mounier Kuhn syndrome has been made. The evolution under
antibiotic treatment (of the episode of infection) and adequate chest
physiotherapy for postural drainage of secretions was marked by clinical
and biological improvement.
Discussion
Mounier Kuhn syndrome is a rare congenital disorder.
It is characterised by a developmental defect in the connective tissue
and smooth muscle resulting in increased tracheal diameter and enlarged
main bronchi. There is also an absence of the myenteric plexus of the
bronchial tree. Diagnosis usually takes place in adulthood. No
correlation between increasing age and increasing tracheal diameter was
found [2].
The syndrome was first described by Mounier Kuhn in
1932 and the term tracheobronchomegaly was introduced by Katz and al. in
1962. The mechanism is not known. It is a rare disease that can come in
congenital form: familial forms were described with possible recessive
inheritance, or in acquired form: Pulmonary fibrosis in adults and after
mechanical ventilation in premature babies (Barotrauma). Some patients
develop mucosal herniation between the tracheal rings leading to
tracheal diverticulosis. The poor clearance of secretions is associated
with recurrent lower respiratory tract infections [3]. There is also
increase in dead space and tidal volume [4].
This syndrome predominates in humans in the third and
fourth decade [5]. Our presentation is that of a 53-year-old patient.
The symptomatology is non-specific, poor or absent and is manifested
basically by recurrent bronchopulmonary infections [6] and it is the
same clinical symptomatology reported in our observation. The clinical
examination can be strictly normal, as it can show nasosinus polyposis
and a polymalformative syndrome with bilateral ptosis, epicanthus,
micrognathia and excess skin of the upper lip. Our patient presents only
bilateral ptosis. Asthenospermia or azoospermia has been reported in
some patients with Mounier-Kuhn syndrome. Chest X-ray can help diagnosis
by showing an increase in the size of the trachea beyond 3 cm
especially in profile incidence [7].
Thoracic computed tomography confirms the diagnosis,
it finds an increase in the tracheal transverse diameter upper than 3cm
in adults, and an increase in the right and left main bronchi greater
than à 2.4cm et 2.3cm respectively. It also serves to reveal cylindrical
or cystic proximal bronchiectasis, extending to the fourth-order
bronchi. The distal bronchial tree is usually normal. Magnetic Resonance
Imaging (MRI) does not have any supplementary advantage in diagnosis
[7].
Bronchoscopy may show dilated proximal airways with
purulent secretions, tracheal diverticula and tracheomalacia. Recent
data would suggest that bronchoscopy with confocal microscopy may aid
diagnosis by permitting real-time analysis of the bronchial mucosal
microstructure, demonstrating a deficiency of elastin fibres within the
bronchial wall. Bronchoscopy can be difficult to perform because of
important airway obstruction due to tracheomalacia [7].
Spirometry can show different degrees of obstruction
or increased residual function [7]. Meunier-Kuhn syndrome has 3
subtypes. In type 1, there is a slight symmetric dilation in the trachea
and main bronchi. In type 2, the dilation and diverticula are distinct.
In type 3, diverticular and saccular structures extend to the distal
bronchi [8]. Our patient is classed in type 2.
Literature reviews have discussed the possibility of
associating Meunier Kuhn’s syndrome with other congenital pathologies
such as Kenny-Caffey syndrome, Maran’s syndrome, hypogammaglobulinemia,
Ataxia-telangiectasia, Ankylosing spondylitis, Brachman-de Lange
syndrome and cutis lax [8,9]. This association makes the understanding
of the mechanism of the occurrence of Meunier Kuhn syndrome more
complicated. Most frequent pulmonary complications are bullous
emphysema, aspergillosis and pneumothorax [7,10]. Our patient has a
Meunier Kuhn syndrome without any other association or complication.
The main differential diagnosis in our observation is
Williams-Campbell syndrome which is a rare condition characterized by
the absence of cartilaginous rings in the sub segmental bronchi,
resulting in dilation of the cystic bilateral bronchi which collapse on
expiration and induce a hyperinflation. It usually affects the bronchi
beyond third division (fourth to sixth order) [11]. The caliber of the
trachea and main bronchi is strictly normal: this concept is
fundamental; it characterizes the Williams Campbell syndrome and allows
to exclude this diagnosis in our observation.
Treatment is based on physiotherapy and appropriate
antibiotic therapy in case of outbreak Infection (which is often the
result of atypical organisms, tuberculous or non-tuberculous
mycobacteria). Prevention of recurrent infections will prevent
progression to irreversible pulmonary fibrosis [12]. Central impairment
excludes any surgical treatment, and the placement of tracheobronchial
prosthesis was reported in advanced cases. Lung transplantation has been
performed in at least two cases of Mounier-Kuhn syndrome, one of who
unfortunately died in the post-operative period.
Conclusion
Mounier-Kuhn syndrome or tracheobronchomegaly is a
very rare condition who’s congenital or acquired origin is still
controversial. The clinical signs are not very specific and; it should
be kept as a differential diagnosis in patients coming with recurrent
lower respiratory tract infections. The radiological diagnosis is easy,
based on a careful analysis of the central airways and pulmonary
parenchyma by CT examination. However, more work must be done in terms
of treatment and follow up of this orphan disease.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images.
Conflicts of Interest
There are no conflicts of interest between the authors and between the authors and the patient.
Disclosure
This case report was written based on clinical observation without any funding.
Authors’ Contributions
Fatima Zahra Mrabet drafted this manuscript under
Hicham Souhi’s supervision. Jihane Achrane, Hanane Ouazzani, Ismail
Rhorfi and Ahmed Abid have made substantial contributions to acquisition
of data.
To know more about Open Access International
Journal of Pulmonary & Respiratory Sciences please click on: https://juniperpublishers.com/ijoprs/index.php

Comments
Post a Comment