Retrospective Analysis of Doxycycline or Bactrim Prophylaxis for Patients with Chronic Obstructive Pulmonary Disease-Juniper publishers
JUNIPER PUBLISHERS-OPEN
ACCESS INTERNATIONAL JOURNAL OF PULMONARY & RESPIRATORY SCIENCES
Abstract
Background: Azithromycin prophylaxis has
shown to decrease COPD exacerbations but led to hearing deficits.
Therefore, there is a need to study other antibiotics as possible
prophylaxis for COPD exacerbations.
Objectives: To evaluate the effectiveness of doxycycline or Bactrim prophylaxis for patients with moderate to severe COPD.
Materials and methods: We studied patients
with moderate to severe COPD who were treated with prophylactic
doxycycline or Bactrim in the fall and winter months along with their
standard COPD therapy. From patient histories, we determined the number
of exacerbations/year and hospitalizations/year prior to and after
prophylaxis. Paired t-tests were used to analyze the data.
Results: 17 patients with moderate to severe
COPD on standard therapy were identified. Prophylactic doxycycline or
Bactrim were added to their treatment regimens as a part of routine
prophylaxis. Patients were on prophylaxis for a period of 6 months per
year. The number of average exacerbations per year decreased from 4.44 ±
4.42 to 1.20 ± 1.0 (n=15, p=0.0047) and the number of hospitalizations
per year decreased from 1.75 ± 1.12 to 0.00 ± 0 (n=5, p=0.0125). The
number of exacerbations per person during the months with prophylaxis
was 1.19 compared with 1.63 exacerbations per person during the months
without prophylaxis (n=16, p=0.24). The antibiotics were well tolerated.
Conclusion: This retrospective analysis
showed a significant decrease in the number of exacerbations and
hospitalizations per year for COPD patients undergoing doxycycline or
Bactrim prophylaxis. This small study suggests the need for a
prospective randomized study evaluating prophylactic doxycycline,
Bactrim or other antibiotics in patients with moderate to severe COPD.
Keywords: COPD, Bactrim,Doxycycline, Antibiotic prophylaxis
Introduction
Chronic Obstructive Pulmonary Disease (COPD) has
become a worldwide epidemic and continues to be one of the leading
causes of morbidity and mortality [1-3]. It is expected to be the third
most common cause of death worldwide by 2020 [2]. In 2000, patients with
COPD accounted for 8 million physician office and hospital outpatient
visits, 1.5 million emergency department visits, 726,000
hospitalizations, and 119,000 deaths [3]. In 2016, the Global Burden of
Disease Study reported the prevalence of COPD as 251 million cases. All
these lead to increased costs at the individual and societal levels.
Frequent exacerbations are associated with a reduced quality of life and
possibly with increased depression and anxiety [4,5]. Many COPD
exacerbations are due to secondary bacterial infections over viral
infections and therefore, preventative treatments with
antibiotics may help improve quality of life of patients, reduce the
number of exacerbations and reduce health care costs [6]. It is reported
that there is almost a two-fold increase in COPD exacerbations during
the winter months [7].
Despite the availability of effective macrolide
prophylaxis, the potential side effects of these antibiotics limit their
long-term use. Therefore, antibiotics like doxycycline and Bactrim can
be considered viable alternatives for prophylaxis against COPD
exacerbations. Doxycycline, a tetracycline antibiotic, has been shown to
possess anti-inflammatory properties in addition to its antibiotic
properties, which could explain its potential effectiveness for chronic
inflammatory diseases such as COPD [8]. Furthermore, it has been shown
to accumulate in the sputum during its use, which may prevent the
colonization of bacteria and the recurrence of acute infections [9].
More recent
studies have shown that doxycycline decreases the production of
Interleukin-8, which is an inflammatory cytokine [10]. Bactrim,
is a combination of Sulfamethoxazole and Trimethoprim (SMXTMP),
has been shown to be an effective prophylactic agent in
diseases such as Chronic Granulomatous Disease (CGD), whereby
the number of life-threatening episodes decreased from every
10 months to every 40 months when put on prophylaxis [11].
It has also been proven effective as prophylactic treatment for
interstitial pneumonia [12].
Because there is little research regarding the potential
effectiveness of different antibiotics with regards to COPD
prophylaxis, this study focuses on the effectiveness of doxycycline
and Bactrim as potential prophylactic agents.
Materials and Methods
We conducted a retrospective study to determine
effectiveness of alternative antibiotics for COPD prophylaxis.
We used patient records to collect all the information needed.
We included chronic COPD patients, falling in the moderate
to severe categories as per the Global initiative for chronic
Obstructive Lung Disease (GOLD) guidelines, with a smoking
history of a minimum of 20 pack years, already on the standard
COPD therapy prior to the introduction of antibiotic prophylaxis
and who received doxycycline or Bactrim prophylaxis for only
6 months in a year. We excluded patients with co-existing lung
diseases (none of our patients had asthma), patients on yearlong
antibiotic prophylaxis. The patients included represented both
genders equally. From the patient histories, the following
variables were collected: sex, age, COPD therapy, FEV1 %
predicted values, treatment taken, antibiotic prophylaxis used
and dates of exacerbations or hospitalizations. We recorded the
number of exacerbations while only on standard COPD therapy
over a 3 year period, and then when they were put on prophylactic
doxycycline (50mg, twice daily) or Bactrim (double strength,
once daily) for 6 months, from October 1st to March 30th, for
the next 3 years. Exacerbations were defined as any worsening
of symptoms or any acute bronchitis episode requiring a course
of antibiotics and/or prednisone. Hospitalizations refer to dates
on which the patient was hospitalized for symptoms related to
COPD. The number of exacerbations and/or hospitalizations
during this time period were recorded and divided by the
number of years of prophylaxis to get average values. Patients
were treated for COPD at four different centers in the Baltimore,
MD and greater-DC areas. Adherence to medications was
checked every 4-8 weeks.
The primary outcomes for this study were measured
as the change in the average number of exacerbations and
hospitalizations per year with and without antibiotic prophylaxis
(i.e. during the 6-month period after the discontinuation of
prophylaxis). The other outcome of interest was the average
number of exacerbations per person during months with and
without prophylaxis.
In this study, the difference in the number of exacerbations
was normally distributed and hence paired t-tests were used for
analysis.
Results
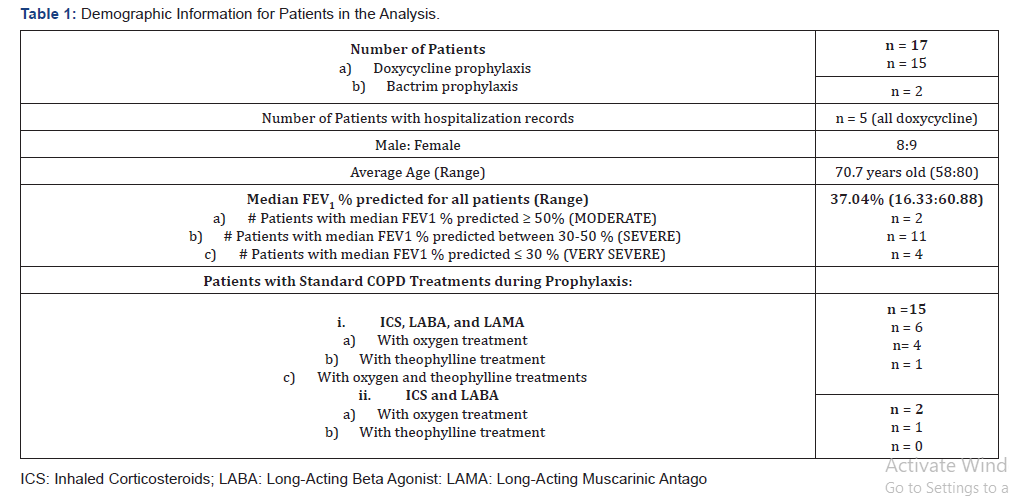
17 patients qualified for the study, with fifteen patients
on doxycycline prophylaxis and two on Bactrim prophylaxis.
Patients were on prophylaxis for 6 months/year for a 3-year
period. The demographic data for the patients with average values for age, FEV1 % predicted and duration of prophylaxis are
reported in Table 1. Most patients were treated with a standard
COPD therapy, which consists of inhaled corticosteroids, longacting
beta-agonists and long-acting muscarinic antagonists.
However, two of the patients were treated without the longacting
muscarinic agonists. Both antibiotics were tolerated well
except for some nausea in thse first few days of doxycycline
treatment. As the prophylactic dose of doxycycline is only half its
therapeutic dose, all the patients reported resolution of nausea
after the first few days.
The number of average exacerbations per year decreased
from 4.44 ± 4.42 to 1.20 ± 1.0 (n=15, p = 0.0034) before
prophylaxis and after the start of prophylaxis respectively
(Figure 1). The number of hospitalizations/years decreased
from 1.75 ± 1.12 to 0.00 ± 0 (n=5, p =0.0125) before prophylaxis
and after the start of prophylaxis, respectively (Figure 1). None
of the patients had reported hospitalizations after they started
the prophylaxis.
The number of exacerbations/people during the months
of prophylaxis was 1.19 ± 1.33 compared with 1.63 ± 2.03
exacerbations/person during the months off prophylaxis (n =16,
p = 0.24). One patient was excluded from this analysis because
she was on yearlong Bactrim prophylaxis.
Discussion
Macrolide antibiotics, specifically azithromycin and
erythromycin, have been shown to decrease the frequency of
exacerbations and to improve the quality of life for patients
with COPD [6,13]. Albert et al. [6] designed a prospective
study, in which subjects received either 250mg azithromycin
or placebo daily. Subjects taking azithromycin had fewer acute
exacerbations than those in the placebo group and the median
time to the first acute exacerbation was significantly longer.
However, adverse side effects such as hearing deficits from longterm
use of azithromycin were reported in a significant number
of patients [6].
We used a retrospective study design, so we did not use a
placebo, instead, we did comparative studies on patients while
on and off prophylactic antibiotics. We chose to administer
antibiotics for a 6-month period during the fall and winter
months (in contrast to previous studies in which patients were
administered antibiotics all year long) since that is when most
exacerbations tend to occur [14].
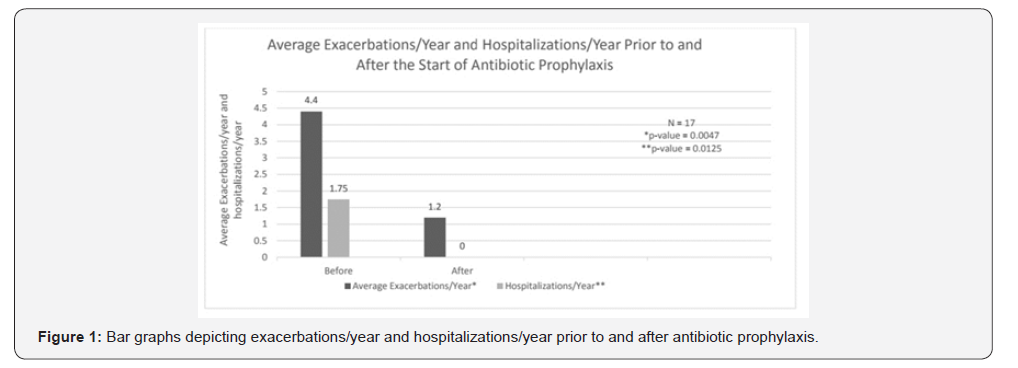
We found that there was a statistically significant reduction
in the number of exacerbations and hospitalizations after the
start of prophylaxis with doxycycline or Bactrim for patients
with moderate to severe COPD (Figure 1). Doxycycline and
Bactrim were tolerated well except for a few cases of mild nausea
in the initial days of treatment with doxycycline. However, our
small study failed to reach statistical significance for the number
of exacerbations and hospitalizations comparing the months
on prophylaxis with the months without prophylaxis. With a
larger study, the results may show a significant reduction of
exacerbations per person during the months when prophylaxis
was taken. This approach of using antibiotics for 6 months a year
instead of yearlong antibiotics may minimize their potential side
effects.
Our study is limited by the small number of study subjects
as well as its retrospective nature. Furthermore, COPD
exacerbations are often not reported to physicians [15]. Not
reporting certain exacerbations could skew the significance of
the data in either direction. Nevertheless, the data reported is
very significant for a small study and supports further studies.
Conclusion
In summary, we retrospectively analyzed the
effectiveness of
antibiotics doxycycline and Bactrim as prophylactic agents for
patients with moderate to severe COPD. From the analysis, these
antibiotics significantly reduced the number of exacerbations/
year and hospitalizations/year. This data supports the need for a
larger, prospective and well-controlled study that can adequately
assess the effectiveness of doxycycline or Bactrim prophylaxis as
alternatives to macrolides, in patients with moderate to severe
COPD. There is a need for studies to determine the effectiveness
of antibiotic prophylaxis specifically in the fall and winter months
versus a yearlong prophylaxis, to compare risks and benefits of
half-yearly prophylaxis as compared to yearlong prophylaxis.
Acknowledgments
We would like to thank Medstar for funding the research.
We would like to thank Georgetown School of Medicine for
organizing the research. We also want to thank the staff of the
Asthma, Allergy and Sinus Centers at Medstar Union Memorial
Hospital, White Marsh, Rockville and Waldorf.
To know more about Open Access International
Journal of Pulmonary & Respiratory Sciences please click on: https://juniperpublishers.com/ijoprs/index.php


Comments
Post a Comment