A Tracheal Web as a Cause of Dyspnea in a Patient who had been treated for Asthma in the Past 35 years-Juniper publishers
JUNIPER PUBLISHERS-OPEN
ACCESS INTERNATIONAL JOURNAL OF PULMONARY & RESPIRATORY SCIENCES
Abstract
A Tracheal Web is a soft tissue formation partially
occluding the trachea lumen. It is of benign origin and can be either
congenital or acquired – the latter mostly in patients with a history of
prolonged intubation. Due to the symptoms that are consistent with
obstructive lung disease, it can often be misdiagnosed as such. As a
result some patients may have been categorized as asthmatics with
minimal response to treatment, since the tracheal web causes a fixed
obstruction pattern. We describe a case of a female 57 year old patient
that had been under asthma treatment for 35 years and was admitted to
Sismanogleio Public Hospital, Greece, due to dyspnea consistent with an
asthma exacerbation.
Laryngotracheal stenosis is a term that refers to a
wide range of clinical conditions that apply to the narrowing of the
airway. It can be of congenital or acquired origin, malignant or benign
[1]. It can cause respiratory symptoms that can be often misdiagnosed as
obstructive lung disease [2-4]. A rare laryngotracheal stenosis subtype
is the tracheal web. We present a case of a 57-year old female patient
with dyspnea who had been diagnosed with asthma since adolescence.
A 57 year old female patient presented to the ER with
symptoms of lower respiratory system infection, probably of viral
origin, and an asthma exacerbation. The patient had been diagnosed with
asthma and allergic rhinitis in the past (35 years ago) and was under
medication with beta 2-agonist and inhaled corticosteroids. She had also
recently been diagnosed with GERD. She was admitted in our clinic for
further investigation and treatment. During her hospitalization she
reported recurrent episodes of shortness of breath and fatigue during
the past years, especially after even mild physical activity. Physical
examination
revealed bilateral inspiratory and expiratory wheezes. Her chest X-ray
was not suggestive of any pathologic findings (Figure 1).

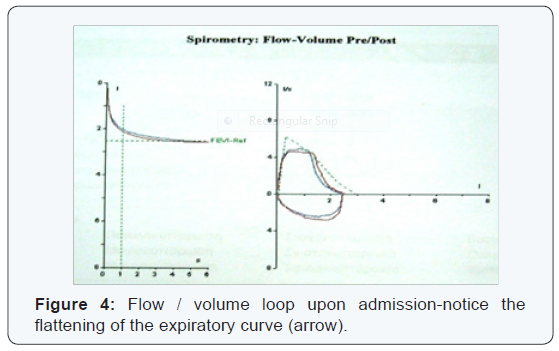
The flow-volume loop demonstated a flattening of the
expiratory flow curve at the PEF level (Figure 4). Until the
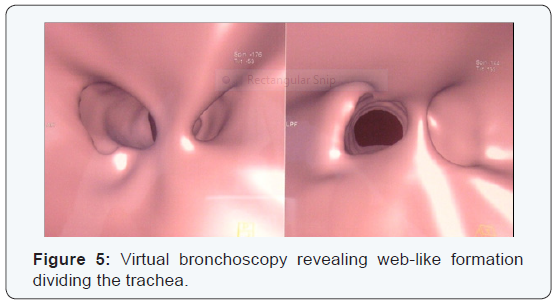
performance status of the patient could allow fiberoptic bronchoscopic evaluation, a virtual bronchoscopy was
performed that revealed web-like formations that divided the
upper trachea in two unequal segments (Figure 5).
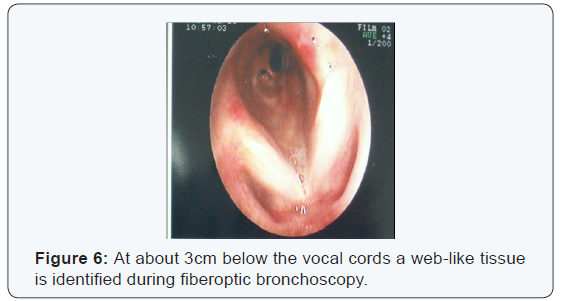
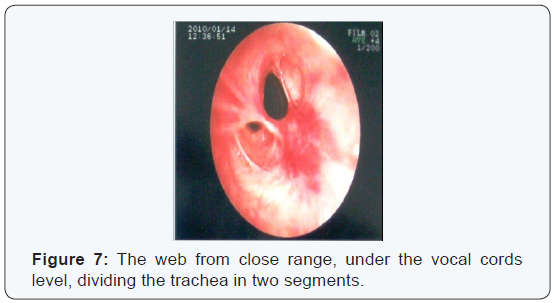
The fiberoptic bronchoscopy that followed had similar
findings; at about 2 cm below the vocal cords a diaphragmatic
lesion was identified, in the form of scar tissue that divided the
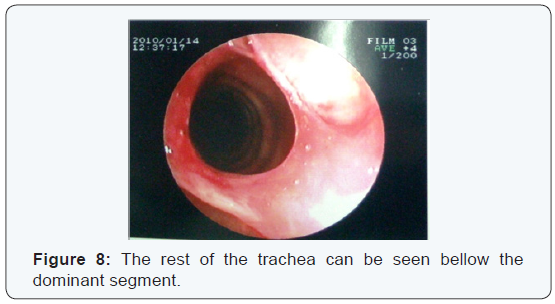
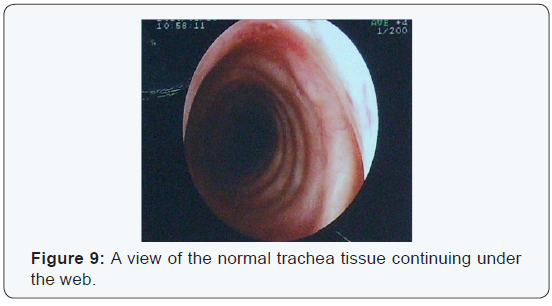
trachea in two parts (Figure 6,7). Beneath the dominant part the
rest of the trachea was normal (Figure 8,9).
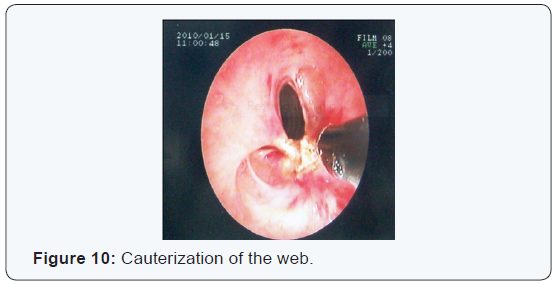
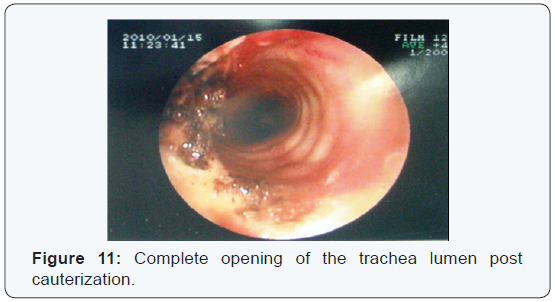
After identifying the lesion, it was removed by means of
electric cauterization with practically complete opening of
the trachea in full diameter (Figure 10,11). The patient was
discharged from the hospital and was programmed for a follow
up bronchoscope and PFT`S in 15 days. The follow up revealed a
normal trachea diameter and significant improvement in PFT`S
(Figure 12,13).


The patient reported a great improvement in her daily
activities, with minimization of dyspnea during exercise and less
need for inhalers. In the next follow up visits her dyspnea had
practically resolved.
Tracheal web is a benign subtype of tracheal stenosis. It
is a rare malformation of the trachea resulting in narrowing
and partial occlusion of the trachea lumen. In most cases it is
congenital, while in adults it is more often acquired as a result
of prolonged tracheal intubation [5]. It consists of soft tissue in
the form of membrane that obstructs partially the trachea lumen
at a level that can vary from intra to extra-thoracic trachea,
thus causing symptoms as expiratory wheeze and/or stridor
depending on the location of the lesion in the trachea lumen [6].
It is a rare condition, with an incidence of 1/104 births in its
congenital form [7].
In some cases the condition is misdiagnosed and the
respiratory symptoms as wheezing, stridor, dysponea and
frequent respiratory tract infections are interpreted as
indicators of obstructive lung disease. This for example may
result in patients diagnosed with asthma that does not respond
to treatment. In other cases the tracheal web is an accidental
finding in adults with no prior symptoms that present an
unexpected difficulty in intubation [8,9]. Differential diagnosis
mainly includes Granulomatosis/polyangiitis, Amyloidosis,
Tracheomalacia, benign tumors (i.e. Characinoid) and complete
tracheal rings. The idiopathic form of tracheal stenosis has a
strong female predominance and has also been associated with
GERD [10].
A strong suspicion of upper airway obstruction can be
taken into consideration if the PFT`S demonstrate a flattening
of the inspiratory and/or expiratory curve with poor postbronchodilator
response, while also important is the high FEV1/
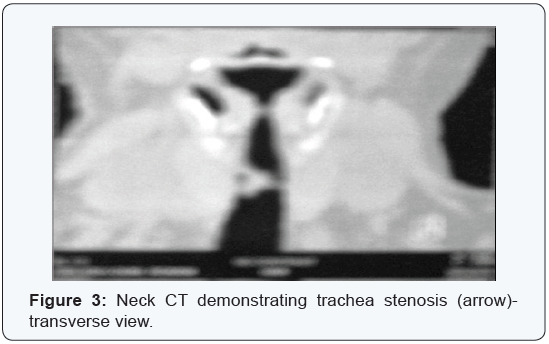
PF ratio [11]. Diagnosis can be achieved by computed tomography
and fibroptic bronchoscopy (gold standard), while the plain CXR
is not usually diagnostic. Treatment is cauterization of the lesion
via fibrotic bronchoscopy and in some cases with cryotherapy
and balloon dilation, with good results and immediate clinical
improvement.
A tracheal web is a condition that membranous soft tissue
partially obstructs the trachea lumen, causing symptoms that
can be misdiagnosed as obstructive lung disease, or in some
cases causing no symptoms but presenting as unexpected
intubation difficulty. In our case we dealt with a female patient
with chronic dyspnea diagnosed with asthma and GERD that had
a fixed obstruction pattern in the flow/volume curve and a poor
response to treatment. The fact that, although diagnosed with
asthma in the past 35 years, her symptoms diminished and her quality of life improved immediately after the bronchoscopic
intervention , should provide food for thought for physicians
who face the challenge of patients with a suspected obstructive
lung disease that demonstrate a fixed obstruction pattern in
PFT`S and poor response to treatment.
To know more about Open Access International
Journal of Pulmonary & Respiratory Sciences please click on: https://juniperpublishers.com/ijoprs/index.php

Comments
Post a Comment