Dynamic Hyperinflation of a Giant Pulmonary Bulla on Single lung Ventilation can cause Cardiac Arrest: A Rare Case-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS INTERNATIONAL JOURNAL OF PULMONARY & RESPIRATORY SCIENCES
Abstract
A 52 year old male presented with history of
progressive shortness of breath, no history of cough or haemoptysis.
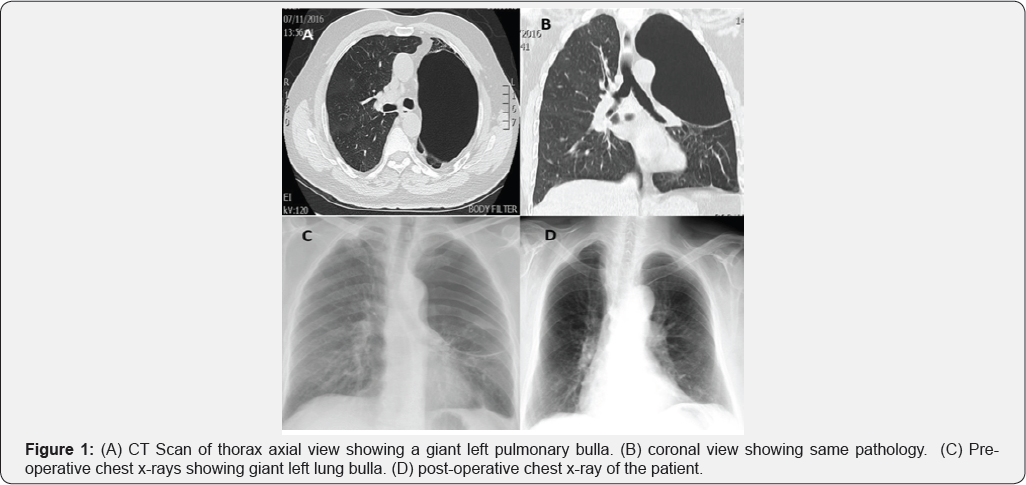
Chest x-ray showed a giant bulla in left hemi thorax. CT scan of chest
revealed a more than half of left hemi thorax occupied by a giant bulla.
Overall both lungs showed emphysematous changes. He was admitted for
video assisted surgical stapling of left lung giant bulla. A double
lumen endotracheal tube was inserted and its position was confirmed with
fibro-optic bronchoscope. While patient was positioned for left
posterolateral thoracotomy suddenly he developed hypotension,
bradycardia and near cardiac arrest. Emergency thoracotomy was
performed, giant bulla which was hyper dynamically inflated because of
mechanical ventilation it was immediately decompressed. Patient was
resuscitated successfully and surgical procedure was completed.
Keywords: Double lumen tube; Single ventilation; Hyper dynamic inflation; Surgery; Cardiac Arrest.
Introduction
Hyper dynamic inflation of the lungs has been
reported in patients with asthma, chronic obstructive airway disease,
emphysematous and transplanted lungs while they are on mechanical
ventilation [1].
Unnoticed progressive hyperinflation of a giant lung bulla can cause
hemodynamic collapse and cardiac arrest. As the change in the
intrathoracic pressure due to hyperinflation is transmitted to great
vessels which results in decrease in venous return to the heart,
hypotension and decrease cardiac output and ultimately leading to
cardiac arrest [2].
Case
A 52 years old man smoker 40/cigarettes per day was
admitted with shortness of breath on exertion, no history of cough, loss
of weight and appetite. His chest X-ray showed a large bulla in left
hemi thorax. Computed tomographic scan (CT) of thorax revealed giant
bullae largely occupying the left hemi thorax (Figure 1).
Routine blood investigations total white cell count, hemoglobin, renal
and liver panels were normal. Preoperative FEV1 was 70%. At room air his
oxygen saturation was 92%. Arterial blood gas analysis showed pH: 7.37,
a PO2 (partial pressure of oxygen) was 65.2mmHg and PCO2
(partial pressure of carbon dioxide) was 50.18mmHg. As the patient was
symptomatic we decided to proceed for bullectomy. Prior to induction of
general anesthesia an emergency surgical instruments trolley was
prepared in case of any inadvertent event.
He was induced with intravenous propofol 2mg/kg and
fentanyl 100 microgram. Muscle relaxation was achieved with intravenous
rocuronium 0.6mg/kg. Double lumen endotracheal tube was inserted after
adequate relaxation. Position of endotracheal tube was confirmed with
fiber optic bronchoscopy to make sure left lung is isolated. Anesthesia
was maintained with oxygen-air (Fio2 0.5) and sevoflurane. Intraoperative monitoring included ECG, Pulse oxymeter, end tidal carbon dioxide (ETCo2),
invasive blood pressure monitoring and temperature. Patient was
positioned for left posterolateral thoracotomy, suddenly patient became
hypotensive BP 60/40, which did not respond to intravenous fluid bolus,
phenylephrine and adrenaline but heart rate continue to slow down up to
10-15 /min. Anticipating the hyper dynamic inflation of giant bullae
compressing the heart emergency thoracotomy through 5th
intercostal space was performed and giant bulla almost occupying the
left hemi thorax was incised for decompression, immediately patient's
hemodynamics start improving, heart rate came back to 100 beat per
minute and blood pressure 100/60 mmHg. Mechanical ventilation was
resumed and double lumen endotracheal tube was repositioned under
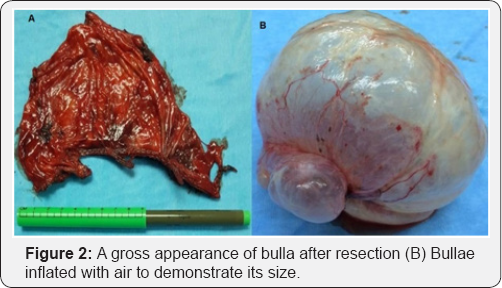
flexible bronchoscopy guidance. Once the patient was stable, bullae were
resected using tristapler and inferior pulmonary ligament was divided
to mobilize lower lobe to fill the hemi thorax (Figure 2).
Chest was closed as a routine in layers and 32Fr chest drain was
inserted. Patient was transferred to ICU and was extubated next morning,
latter on he was transferred to the ward. He was discharged for further
follow up in outpatient.
Discussion
Double lumen endotracheal intubation for single lung
ventilation is required in a lot of thoracic surgical procedures for
better surgical exposure and protection of contralateral lung from
contamination and spillage of blood in case of hemoptysis. Single lung
ventilation is very challenging for the anesthetist to maintain the
oxygenation and hemodynamic stability throughout the surgical procedure,
as this creates a large intrapulmonary shunt which can cause hypoxia
and end organ damage. Excessive positive end expiratory pressure,
hypoxia, hypercarbia and hypovolumia may contribute to high pulmonary
vascular resistance of dependant lung which increase the shunt fraction.
Different sizes of double lumen tubes are available ranging from 27F to
41F. Correct size of double lumen tube almost completely seal the
bronchial lumen without inflation of cuff. Small tube with high
inflation pressure and large tube in small bronchus can cause mucosal
damage [3].
Anesthesiologist confirms the correct position of endotracheal tube
with bronchoscopic examination. As this has proved that 48% of tubes are
usually malpositioned, which is very hazardous. Apart from difficult
surgical exposure this can cause impaired ventilation, hypoxia, gas
trapping, pneumothorax and contamination of other lung [4].
Pulmonary bullae are abnormal dilatation of air spaces distal to
terminal bronchiole and are greater than two centimeter in distended
state. When the bullae occupy more than half of the hemi thorax they are
called giant bullae and commonly seen in patients with paraseptal
emphysema and progressive fibrotic lung disease [5].
These bullas can remain asymptomatic they are treated conservatively.
Surgical treatment is reserved for giant bullae occupying more than
thirty percent of hemi thorax causing compression of adjacent healthy
lung to the extent that patient is having incapacitating dyspnea or
associated complications like, infection, hemorrhage rupture of bulla
leading to pneumothorax [6].
In patients with bullous lung disease induction of general anesthesia
and proper placement of double lumen tube, maintaining hemodynamic
stability and blood gas chemistry throughout the surgical procedure is
difficult task. Such patients need high airway pressure and large tidal
volume to maintain normal arterial carbon dioxide partial pressure which
is injurious to the lungs. General anesthesia and endotracheal
intubation in patients with emphysematous and bullous lung disease can
cause hyper dynamic inflation and enlargement of bullae leading to
cardiovascular compromise and cardiac arrest. Rarely this clinical
condition is diagnosed in early stage usually they are diagnosed late or
on autopsy reports [7,8].
The main contributing factors to cause hyper dynamic inflation are a
large tidal volume, short expiratory time before the next breath is
initiated and chronic obstructive airway disease. When minute
ventilation is higher to prevent passive exhalation of delivered tidal
volume within the given expiratory period, this may create a dynamic
hyperinflation and increased auto peep [9,10].
Pathophysiological consequences of this are deleterious both on the gas
exchange and cardiovascular system. Distended bullae compress the
residual lung leading to compression of alveoli and pulmonary
capillaries which impair the gas exchange due to increase in dead space [11].
As bulla size increases with each breath the
intrathoracic pressure rises too, which compress the big veins and
eventually reduce the cardiac out leading to cardiac arrest. Furthermore
due to giant size and hyper dynamic inflation pulmonary vascular
resistance and right ventricular after load increases this compromises
the left ventricular function. Hyper dynamic inflation should be
suspected if there is sudden hypotension, oxygen desaturation, pulses
paradoxes and distended neck veins when patient is connected to
mechanical ventilation after induction of anesthesia. Although few
methods have been reported in medical literature to quantify the
hyperdynamic inflation including if there is persistent expiratory flow
at the end of expiration on flow volume loop, collecting expired gas in
ventilator bellow, increased peak and plateau pressure during volume
controlled ventilation decrease in tidal volume during pressure
controlled ventilation and increase in auto peep. None of these methods
is perfectly accurate and applicable [12,13].
Dynamic hyperinflation can be prevented by early
recognition and ventilator manipulation to adjust low tidal volume, low
respiratory rate and inspiratory, expiratory ratio that favors prolonged
expiration. During perioperative period permissive hypercarbia and
hypoventilation without compromising the FiO2 is a common practice. High
PEEP is dangerous in such cases. Nitrous oxide should not be used
because this is 34 times more diffusible than nitrogen and can lead to
expansion of air- filled cavities.
Conclusion
Early recognition and immediately disconnecting the
patient from ventilator and emergency thoracotomy and decompression of
bullae with pharmacological support for the near cardiac arrest saved
his life. Early recognition of hyper dynamic inflation of giant lung
bulla is very important as this can lead to signific hemodynamic
instability and may precipitate cardiac arrest,which may ultimately
cause death.
To know more about Open Access International
Journal of Pulmonary & Respiratory Sciences please click on: https://juniperpublishers.com/ijoprs/index.php
To know more about Open access Journals
Publishers please click on : Juniper Publishers
To know more about juniper publishers: https://juniperpublishers.business.site/

Comments
Post a Comment