Lung Cancer; Approaches for Immunotherapy and Immune Chemotherapy-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS INTERNATIONAL JOURNAL OF PULMONARY & RESPIRATORY SCIENCES
Abstract
Lung cancers are one of the most frequent cancer and
causing death for both men and women in the world. Through the
acceptance of novel biomarkers, it has been possible to recognize
subsets of patients who reap the benefits of targeted molecular
solutions. The success of targeted anticancer remedies and new
immunotherapy methods has created a fresh paradigm of personal therapy
and has also led to accelerated development of new drugs for lung cancer
treatment. In addition to, recently Monoclonal antibodies to programmed
death 1 and its ligand are now approved for both first and second brand
treatment patients with metastatic lung cancers. In this Summary, we
will put together the explanation and current research strategies
looking into the role of immunotherapy and immune chemotherapy in
resectable non-small cell lung cancers (NSCLC), as well as potential new
targets for drug development.
Introduction
Like all malignancies, Cancers of the lung, results
from an abnormal proliferation cells in the body. Normally, our body
maintains a system of mounts and inspections on cell progress so that
skin cells divide to produce new cells only when new organ cells are
needed. Disruption of this system of assessments and balances on cell
development results within an uncontrolled division and proliferation of
cells that eventually forms a mass known as a hyperplasia and may will
progress to neoplasia [1].
Three main types of lung cancer; knowing which kind we have important
since it affects our treatment options and your perspective (prognosis).
These include small cell lung cancers (SCLC), non-small cell lung
malignancies (NSCLC) and lung carcinoid tumor.
About 85% of lung cancers are NSCLCs, 10%-15% SCLC
and less than 5% lung carcinoid tumor. The level of lung malignancy
refers to the level of spread in the body. In addition, lung cancer cell
can spread to other organ in the body, certain locations particularly
the adrenal glands, liver, brain, and bones are the most frequent sites
for lung malignancy metastasis [2].
Also the lung is a very common site for metastasis from malignant
tumors in other parts of the body. Reports from the North American
Cancer Society predicted that in 2018 we will see about 244,000 new
cases of lung cancer tumor in the U.S.A [4]
and over 154,000 fatalities of disease. Lung cancer tumor is
predominantly an illness of older people; almost 70% of people diagnosed
with lung tumor are over 65 years, while it is less than 3% of lung
malignancies occur in people under 45 years. The median get older at
identification is 70 years [5]. Treatment of lung tumor can require a combination of surgery, chemotherapy, targeted remedy, immunotherapy, radiation therapy
Different malignancies have different risk factors.
Some risk factors, like smoking, can be altered the cell to hyperplasia.
Others, like an individual's age or family background, cannot be
changed [6].
But having a risk factor does not mean that you will get the disease.
And a lot of people who get the disease may have few or any known risk
factors. Some risk factor can be changed include: Cigarettes smoke,
exposure to the product, Arsenic in drinking normal water and certain
health supplements. And some risk factor are unable to changed include;
air pollution, Personal or family history and ancestors of lung cancer
and factors with unsure or unproven effects on lung cancer risk such
Smoking marijuana and Talcum powder [7].
Lung Cancer Biomarkers
Biomarkers are simply just defined as components we
can use to distinguish abnormal from normal status .In the recent years,
the molecular abnormalities in a sizable proportion of patients has
allowed the emergence of individualized targeted remedies and has opened
new horizons and created new expectations for these patients [6].
The use of predictive biomarkers to identify tumors that may respond to
targeted treatments has meant an alteration in the paradigm of lung
cancers diagnosis [7].
It has been possible to identify subsets of patients who reap the
benefits of targeted molecular therapies. The success of targeted
anticancer solutions and new immunotherapy approaches has created a new
paradigm of personalized therapy and has also led to accelerated
development of new drugs for lung cancer tumor treatment. Table 1
includes cancers biomarkers as targets for therapy. Malignancy
biomarkers can consist of most biomolecules used for medical purposes,
including protein, genetic materials such as DNAs, methylated DNAs,
RNAs, and microRNAs (miRNAs), oligosaccharides, lipids, and metabolites,
because tumor is a heterogeneous disease that display gene and health
proteins changes in a cancer cell [8,9].
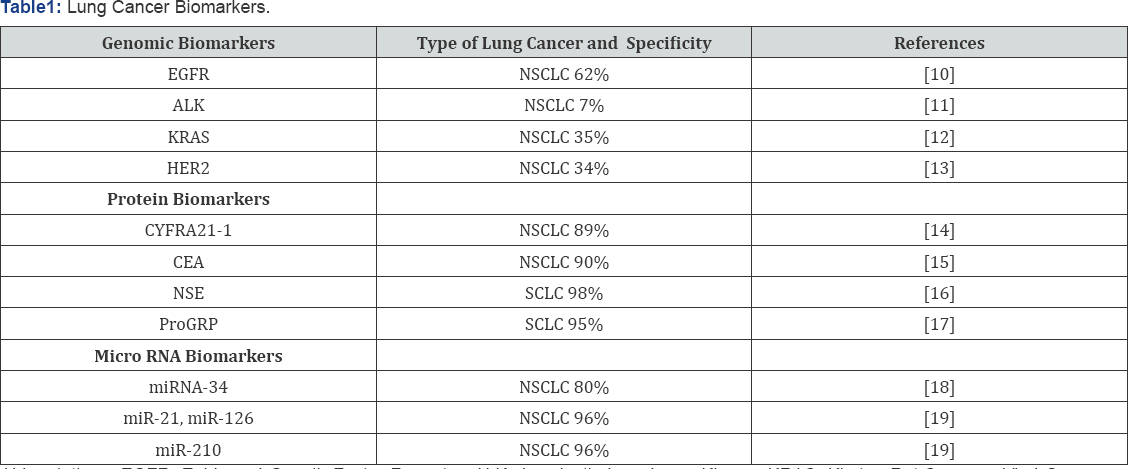
Abbreviations: EGFR: Epidermal Growth Factor
Receptor; ALK: Anaplastic Lymphoma Kinase; KRAS: Kirsten Rat Sarcoma
Viral Oncogene Homolog; HER2: Human Epidermal Growth Factor Receptor 2;
CEA: Carcinoembryonic Antigen; CYFRA21-1: Cytokeratin 19 Fragment, NSE:
Neuron-Specific Enolase; ProGRP: Progastrin-Releasing Peptide
Immunotherapies for Lung Cancer
Nonspecific immunotherapy for lung cancer
The efforts of nonspecific immune system stimulation-
based therapies have yielded equivocal results. The properties of lung
tumors to evade immunosurveillance is a result of the creation of
immunosuppressive chemokines of the tumor cells, loss of MHC antigen
manifestation, and higher amounts of T-regulatory (Treg) the tumor
microenvironment [20,21].
However Restorative vaccines have been used to top rated the host
disease fighting capability to recognize tumor antigens and augment
antitumor T-cell reactions; two types of vaccines are being examined in
NSCLC: tumor cell and antigen-based vaccines[22].Immunization
against tumor epitopes (alternative splicing peptides) is attained by
injections of recombinant tumor antigen proteins, peptides, or
gangliosides that subsequently activate humoral and mobile immune
replies against tumor antigens[23].Immunotherapy
uses both dynamic and passive replies of the immune system to treat
various kinds of malignancy. Although immunotherapeutic brokers have
been approved for quite some time now to treat such cancers as melanoma
and lymphoma, NSCLC was at one time considered nonimmunogenic or not
susceptible to immune- mediated killing of cancer cells, mostly because
of failed attempts at immunomodulation with interleukin-2, interferon,
and Bacillus Calmette-Guerin. However, clinical advances have led to the
creation of immunotherapies that ease the suppression of antitumor
activity in a number of cancers, including situations of advanced NSCLC [24].
Productive immunotherapy modulates the disease fighting capability and
has been classified as nonspecific and specific, the previous of which
is seen as a general immune system response and the latter of which
consists of the stimulation of humoral and cell- mediated immunity.
Examples of active immunotherapeutic real estate agents include
recombinant cytokines, bio chemotherapy, cancer vaccines, and
immunomodulatory monoclonal antibodies[25].
On the other hand Immune checkpoints make reference to inhibitory
pathways vital for retaining self-tolerance; tumors use certain
checkpoint pathways to escape immune surveillance[26].
Inhibitory ligands and receptors that regulate T-cell effectors
functions are generally overexpressed in tumor skin cells or in the
tumor microenvironment. Then, the blockade of immune checkpoints
releases the breaks on the immune system leading to antigen-specific
T-cell replies.
Specific Immunotherapy for lung cancer
Chemotherapy to surgery as adjuvant or neoadjuvant
treatment can improve success rates by about 5% at 5 years. Lately,
major developments in cancer tumor immunotherapy have resulted in better
outcomes for most patients with lung cancers. Immunotherapy has used
immune system cells or monoclonal antibodies for stimulated immune
system [27].
Monoclonal antibodies to programmed death 1 and its ligand are now
approved for both first and second range treatment patients with
metastatic lung malignancy. Lately, treatment with immunotherapy ligands
(programmed cell death-1)PD_1, PD-L1 and (T-lymphocyte-associated
antigen-4)CTAL-4 can improve final results compare to chemotherapy for
NSCLC patient in the metastatic setting has leading lots of clinical
trials.in addition to, immunotherapy has less toxicity than compared to
cytotoxic chemotherapy [28]. Peruse analysis showed that immunotherapy evolved immunosuppressive microenvironment in lung tumors[29].Furthermore,
the Researchers has shown PD1/PDL1 inhibitor remedy for advanced NSCLC
has a significantly higher objective response rate (ORR) and a higher
rate of immune system-mediated pneumonitis when used in front-line
setting when compared with chemotherapy cared for patients. Various
anti-PD-1/PD-L1antibodies are already approved for the first- and
second-line setting up. There are a number of monoclonal antibody for
inhibits PD1 like: Nivolumab and pembrolizumab and for PDL1 inhibit
atezolizumab that Food and Medicine Supervision (FDA) approved
treatments for patients with NSCLC[30]
. However ipilimumab, is available to prevent the binding of CTLA-4
with its ligands (CD80/CD86), resulting in reactivation of the antitumor
immune response mediated by specific T cells[31].
Peruse study validated the NSCLCs exhibit and exposed
PD- L1 for inhibit function effect or T skin cells in microenvironment
tumor. Then, T adapted treatment of cancer tumor cells not very
successful. In this regard, scientific studied and looked into for
outcome this problem. Nonetheless, PD-L1 manifestation has been
associated with EGRF mutation, which has been reported to correlate with
a higher likelihood of respond to PD-1 blockade, recommending that
immunotherapy in EGFR-mutant NSCLC may still maintain promise.
Osimertinib is an oral, third-generation, irreversible epidermal growth
factor receptor tyrosine kinase inhibitor (EGFR-TKI) that selectively
inhibits both EGFR-TKI- sensitizing [32].
Osimertinib proved efficacy more advanced than that of standard
EGFR-TKIs in the first-line treatment of EGFR mutation-positive advanced
NSCLC, with an identical safety profile and lower rates of serious
negative events. Then, recently immunotherapy has success options for
treating cancer therapy
Proposed Immune chemotherapy for lung cancer
Current work are concentrating on new potential
combination strategies with synergistic antitumor activity, using immune
checkpoint blockade as a partner for targeted real estate agents and
toxin conjugate anti PDL1 and lead toxin to internalize inside tumor
cell [33].
Tumor cell death brought on by chemotherapeutic and targeted agencies
strengthens the antitumor immune response by release of neoantigens.
This offers a unique opportunity for combo strategies with synergistic
antitumor activity, using immunotherapy as a partner for chemotherapy,
targeted brokers and other immune system checkpoint inhibitors [34].
Herein we discuss the available data on the blended use of
immunotherapy, including PD-1/PD-L1 and CTLA-4 inhibitors, with EGFR and
ALK inhibitors and touch upon the current status of immunotherapy plus
antiangiogenic drugs for molecularly unselected advanced NSCLC.
Antiangiogenic providers focusing on the vascular endothelial progress
factor (VEGF) and VEGF receptor (VEGFR) have also reshaped the approach
to the treatment of advanced NSCLC. For instance: A period review of
ipilimumab in combination with chemotherapy in patients with advanced
NSCLC revealed very promising results, with a significant improvement in
PFS versus a control group cured with chemotherapy only [34].
On the other hand, among the important portion of the immune system,
cytokines play an integral role in tumor suppression, which induce
functional immune cell proliferation and the secretion of inflammatory
cytokines to eliminate cancer cells [35].
Cytokine treatments have been applied extensively in various solid
tumor and lymphadenoma due to their favorable curative effect [36].
Recently, many studies have been conducted on the blend of cytokines
and chemotherapy, that could cause activation of the innate disease
fighting capability and inhibit the tumor expansion more proficiently [37,38].This
combined immune-chemo treatment against cancer may start a new way for
improved cytokine remedy in cancers treatment. For instance: investigate
the anti-cancer effects and mechanisms of immunochemotherapy of
5-fluorouracil (5-FU) and interleukin-2 (IL-2) on non-small cell lung
cancer tumor (NSCLC) A549 cells. Combination remedy significantly
inhibited tumor growth in comparison with monotherapy with 5-FU or IL-2
and enhanced the identification and lysis of tumor cells by NK skin
cells. 5-FU and IL-2 immunochemotherapy significantly inhibited tumor
development and turned on NK cytotoxicity in vivo. Therefore, all of the
data suggested that combo immunotherapy and chemotherapy may provide a
new treatment option for patients with lung tumors [39].
Conclusion
Immunotherapy with monoclonal antibodies to PD-1 and
PD- L1 are now approved for treatment of patients with metastatic NSCLC,
and also have been shown in several randomized tests to lead to raised
outcomes for select patients in comparison to standard chemotherapy.
Studies are currently underway evaluating the safest and most effective
ways of combine these treatments in the multi-disciplinary management of
patients with resectable NSCLC. Studies with additional immunotherapy
realtors, including combo immunotherapies, chemo- immunotherapy, and
CAR-T cells, will build on our current understanding and add ideally
yield new treatments that lead to better final results for patients with
early-stage NSCLC.
To know more about Open Access International
Journal of Pulmonary & Respiratory Sciences please click on: https://juniperpublishers.com/ijoprs/index.php
To know more about Open access Journals
Publishers please click on : Juniper Publishers

Comments
Post a Comment