Contribution of Computed Tomographyin The Diagnosis of Pulmonary Tuberculosis at Kiffa Regional Hospital, Assaba-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS INTERNATIONAL JOURNAL OF PULMONARY & RESPIRATORY SCIENCES
Abstract
Background: Computed tomography (CT) is
currently the most sensitive and specific medical imaging examination
for lung diseases, but it’s use should be based on the results of
clinical examination and chest X-ray.
Objectives: This study aimed to describe the
contribution of CT in the diagnosis of pulmonary tuberculosis (TB) in
symptomatic patients with normal chest X-ray.
Materials and methods: This was a prospective
study conducted in 2017 in Kiffa Regional Hospital, Mauritania, in
patients requiring a chest X-ray for suspected pulmonary TB. CT imaging
was performed if sputum examination was negative and chest X-ray was
normal.
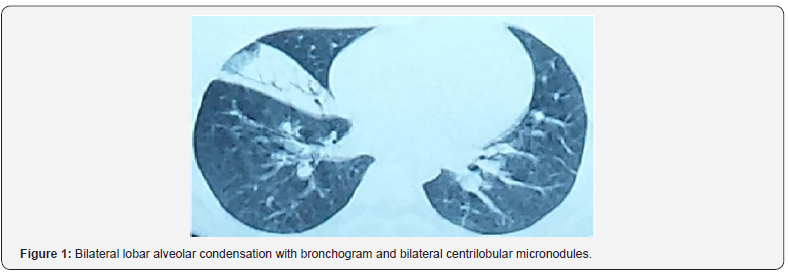
Results: Twenty-four TB cases (mean age, 43.7
years; sex ratio M/F, 2.0) were included. The presenting symptoms
included chest pain (79%), chronic cough (71%), fever (63%), and dyspnea
(46%). CT imaging showed medium lobar alveolar condensation with a
bilateral centrilobular and micronodular bronchogram (13%), interstitial
anomalies in the form of numerous inter- and intra-lobular pleural
cross-links in the middle and lower right lobar lobes (25%), diffuse
fibrotic interstitial pneumopathy (17%), and micronodules, confluent
nodules, condensations, and unilateral cavities (42%).
Conclusion: CT is particularly valuable for
tracking and monitoring parenchymal nodules, for establishing the
diagnosis and monitoring of infectious pneumonitis, secondary thoracic
complications, and exploration of unexplained lung disease. Although
chest radiography has several shortcomings to establish the diagnosis of
TB in patients who have negative sputum smears, it is still useful for
initial screening. For cases with clinical signs of active disease and
normal chest X-ray, CT is indicated.
Keywords: Pulmonary tuberculosis; Radiography; Scanography; Mauritania
Introduction
Tuberculosis (TB) is a public health problem
worldwide, especially in developing countries. The persistence of
tuberculosis is partly related to increased longevity and aging of the
population and emergence of drug-resistant Mycobacterium
tuberculosisstrains [1]. In resource-limited settings where sputum
culture and nucleic acid amplification techniques are not routinely
available, diagnosis of pulmonary TB is based on clinical signs and
symptoms (fever, productive cough, purulent sputum, hemoptysis, dyspnea,
weight loss, loss of appetite),
microscopic examination of sputum smear, and chest X-ray [2]. An
additional difficulty is that the diagnosis can be difficult when signs
and symptoms are either atypical or non-specific, such as acute
pneumonia, chroniccough, fever, and diarrhea. Autopsies in several
countries have shown that an accurate diagnosis of pulmonary
tuberculosis was made in only about 50% of cases [1-5]. In many cases,
diagnosis is established too late, allowing the spread of contagion from
undetected cases. In countries where both tuberculosis and Human
Immunodeficiency Virus (HIV)/ Acquired Immunodeficiency Syndrome (AIDS)
are endemic, HIV testing is essential in all patients with tuberculosis.
A sociological difficulty also lies in the fact that diagnostic
approaches of these two diseases are historically different.
Anti-tuberculosis campaigns have been public, whereas HIV/AIDS screening
is generally individual and confidential in many countries. It has been
reported that currently only about 10% of Africans are suffering from
pulmonary tuberculosis [3].
In industrialized countries, Computed Tomography (CT)
tends to replace traditional diagnostic methods not only to establish
the definite diagnosis of TB, but also to monitor the evolution of the
disease. Most often, the radiographic images in a standard chest X-ray
are quite suggestive of pulmonary TB. However, patients in whom chest
X-rays present atypical features that confound interpretation of the
radiographic images would benefit from the high-resolution CT imaging.
Although CT has the advantage of providing a more accurate imaging, the
cost involved in the acquisition and maintenance of the equipment and
patient charges may be too high, especially in less developed countries
where the incidence of TB remains high. Within this context, it is
essential to determine the place of CT to establish the diagnosis of
pulmonary TB in Mauritania. The aim of the present study was to compare
CT to standard chest radiography in establishing TB diagnosis.
Materials and Methods
This was a prospective study conducted in Kiffa
Regional Hospital from January 1 to December 31, 2017, in all patients
requiring a chest X-ray. Diagnosis of pulmonary TB was performed on an
ambulatory basis, except in patients presenting severe signs and
symptoms (hemoptysis, altered consciousness) who were hospitalized.
Three sputum samples were collected from all patients with suspected
pulmonary TB. Patients were included after informed consent if (i) they
had been treated unsuccessfully with non-specific antibiotic therapy,
(ii) had at least three negative microscopic examinations of sputum
specimens, (iii) but presented X-ray and/or CT evidence of TB, and (iv)
responded favorably to anti-tuberculosis therapeutic test. Patients with
positive sputum smears or radiological abnormalities and treatment
success with non-anti-TB antibiotics were excluded. All CT scans were
reread blindly by an experienced radiologist to identify parenchymal
lesions and theirbronchial, mediastinal, pleural and parietal
morphology.
Patients were screened for HIV by ELISA, and the
results were confirmed by Western blot. For each patient, clinical and
epidemiological data (age, sex, geographical origin) and history of
anti-TB treatment and evolution of the disease (i.e., the results of
sputum smears after 2, 3, 5 and 6 months of treatment) were collected
and recorded. The anti-TB treatment for all patients consisted of the
combination regimen rifampicin (10 mg/kg/day), isoniazid (5 mg/kg/day),
ethambutol (20 mg/kg/day), pyrazinamide (30 mg/kg/day) for two months,
followed by dual therapy with rifampicin and isoniazid for four months
at the same dosages.
Results
During the period of twelve months, 24 patients who
met the inclusion criteria were included. The study focused only on
patients who were able to perform both chest X-ray and thoracic CT. The
mean age was 43.7 years (range, 15-76 years). The sex ratio of men to
women was 2.0. The majority of our patients (20/24, 83%) came from rural
areas. The mean time to diagnosis was seven weeks, with general signs
dominated by chest pain (79%), chronic cough (71%), fever (63%), and
dyspnea (46%). Other presenting signs and symptoms included hepatomegaly
(38%), general impairment (25%), polyadenopathy (17%), and hemoptysis
(13%). Chest X-ray in these patients was normal. The following CT
abnormalities were observed, in decreasing order: medium lobar alveolar
condensation with a bilateral centrilobular and micronodular bronchogram
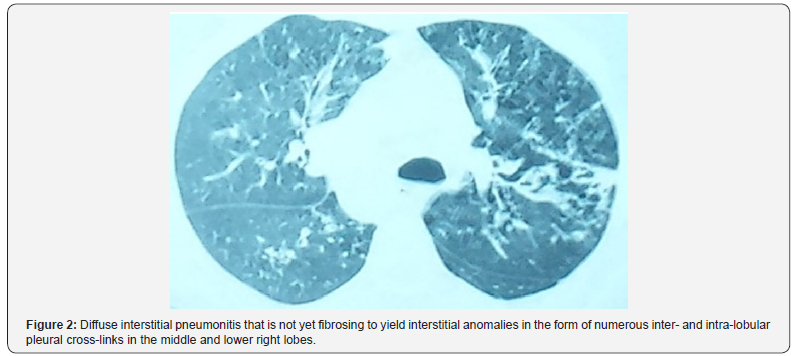
(Figure 1) (3cases of 24 patients, 13%), interstitial anomalies in the
form of numerous inter- and intra-lobular pleural cross-links in the
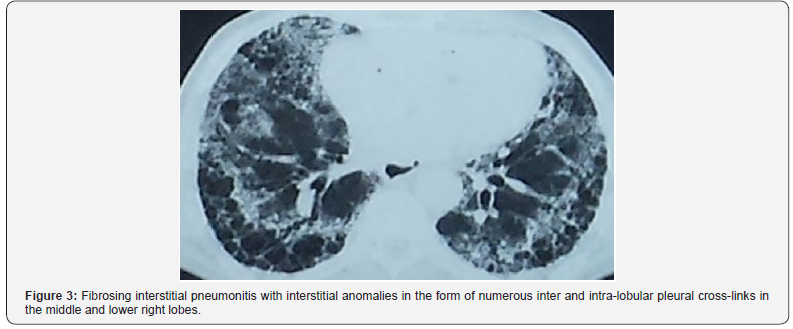
middle and lower right lobar lobes (25%) (Figure 2), diffuse fibrotic
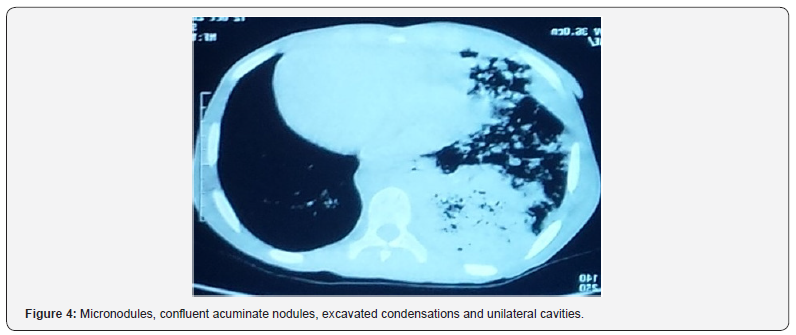
interstitial pneumopathy (17%) (Figure 3), and micronodules, confluent
nodules, condensations, and unilateral cavities (42%) (Figure 4).
Bacteriological examination of the sputum for M. tuberculosis and HIV
serology were negative in all patients.
Discussion
TB is still one of the most common infectious
diseases in the world. It is the second leading cause of death due to
infectious disease worldwide [4-6], especially in the developing world,
after HIV [5-8]. In Mauritania, the limited diagnostic capacity of TB
remains a challenge to improve case detection rates. The clinical
diagnosis of this serious disease is difficult. Laboratory diagnosis
(sputum examination) and chest X-ray are often required to establish the
diagnosis. The demonstration of a radiological parenchymal infiltrate
is a strong argument in its favor. Early diagnosis of pulmonary TB is
not always easy to establish since very often it shares non-specific
radiographic changes with the more common pathological pneumopathies,
leading to late diagnosis [9]. In our study, the average time to
diagnosis was 7 weeks, with chest pain, chronic cough, fever, and
dyspnea as the most common signs and symptoms. The time to diagnosis and
presenting signs and symptoms were similar to those reported by other
African authors [7-9]. Initial chest X-rays performed in our patients
were normal. Other authors have observed that chest X-ray may be normal
in 15% of smear-positive TB patients [10]. Radiologically, pulmonary TB
is typically characterized by parenchymal, ganglionic, pleural or rarely
diffuse hematogenous pulmonary involvement [11]. Although microscopic
examination of sputum is commonly practiced, in many developing
countries, chest X-ray remains a standard diagnostic tool for pulmonary
TB. However, chest X-ray is inadequate in 30 to 40% of cases [12]. Chest
X-ray has low sensitivity and low specificity and may show images of
parenchymal abnormalities with delay.
Our study provides the first CT data from patients
with smear-negative pulmonary TB in Mauritania. Indeed, the role of
radiographic imaging in the diagnosis and monitoring of pulmonary TB is
crucial. Most often, the aspects and morphology seen in radiographic
images of lesions are suggestive of TB. However, in “radiographically
silent forms,” CT can provide images of thin sections in high resolution
and reveal ‘cryptic’ TB. In restricted circumstances, CT becomes an
essential diagnostic tool to identify radiographically negative patients
with active TB [13]. An early performance of a chest CT scan can have
an important impact on case management in such cases [12,13]. However,
due to the high cost of purchase and maintenance of CT scan, especially
in a country where the incidence of TB remains high, it is essential to
determine the most appropriate place of CT in establishing the diagnosis
of pulmonary TB. The present prospective study performed over 12 months
was limited to 24 radiographically negative patients with confirmed
pulmonary TB who benefited from CT scan. The mean age, sex ratio, and
origin of our patients were comparable to those of a previous study
conducted in the same region in Mauritania [7].
CT has become an essential complementary examination
in the exploration of thoracic and especially parenchymal pathologies.
In our case series, CT abnormalities have been dominated by images of
lobar and micronodular alveolar condensation. CT is more sensitive to
detect micronodules, determine their random diffuse distribution at the
pulmonary level, and detect small lesions which may be located in areas
that are poorly explored in standard radiography, such as the pulmonary
apex (area of particular interest in the study of tuberculosis) and also
subpleural, juxta-mediastinal and juxta-diaphragmatic regions. CT thus
makes it possible to evaluate the signs of activity of the disease, to
better detect the evolution of complications and sequelae, to guide the
location of biopsy samples in atypical forms, making it possible to
avoid thoracotomies, and to follow the evolution of lesions under
treatment [12].
However, CT scan has several limitations which are
mainly represented by its radiating nature, the need in some cases for
an injection of ioversol contrast medium, and the need for cooperation
of the patient who must remain immobile and in apnea during imaging,
which is difficult to attain in children and agitated patients. These
limitations may sometimes cause the examination to be deferred or
substituted by another technique [14,15]. One of the major limitations
of CT is the examination of the mediastinum. Indeed, its analysis
requires an injection of contrast medium and a higher irradiation dose
because the spontaneous contrast of the mediastinal structures is weak.
Thus, the irradiation of an examination of the mediastinum cannot be
reduced as much as that of an image acquisition of the pulmonary
parenchyma. As a result, the scanner is too small to be currently
adapted to the research and analysis of mediastinal pathologies, even if
it allows a rough visualization of the main anatomical structures. A
second major limitation of the dose scanner is related to the morphotype
of the patient. The more corpulent a patient is, the more X-rays will
be absorbed, and the poorer will be the quality of the image. Thus,
beyond a certain weight, the poor image quality may compromise the
establishment of the correct diagnosis. Another limitation of CT is the
difficulties in the analysis of interstitial parenchymal abnormalities.
Indeed, the CT abnormalities encountered in diffuse interstitial
pneumonitis are subtle, especially in the initial phase when the main
lesions are sometimes not very distinct [14]. Despite these limitations,
CT imaging may be helpful in certain circumstances to diagnose TB.
Conclusion
In Mauritania, the prevalence of TB is still high,
and the diagnosis of TB with negative bacteriological examination
remains difficult because of the insufficiency of the technical platform
and limited financial resources of patients. From a pragmatic
perspective, the diagnostic approach usually consists of clinical
examination and chest X-ray. However, for diagnostic confirmation,
bacteriological and/or histological examinations are required. Although
the standard chest X-ray remains the reference diagnostic method in most
cases, CT may be crucial in some cases for the diagnosis and monitoring
of pulmonary TB.
Declaration of Transparency
The authors have no conflict of interest to declare.
Acknowledgments
We are grateful for the tireless efforts of the medical staff for their excellent patient care at Kiffa Regional hospital.
To know more about Open Access International
Journal of Pulmonary & Respiratory Sciences please click on: https://juniperpublishers.com/ijoprs/index.php
To know more about Open access Journals
Publishers please click on : Juniper Publishers

Comments
Post a Comment