In Vitro Preparation of H2O2 Inactivated Rabies Vaccine and Related Immunogenicity-Juniper publishers
JUNIPER PUBLISHERS-OPEN ACCESS INTERNATIONAL JOURNAL OF PULMONARY & RESPIRATORY SCIENCES
Abstract
The aim of the present work is to produce local H2O2 inactivated vaccine and monitor its quality to the currently available in the Egyptian market. Data revealed that H2O2
could inactivate rabies virus within 3 hrs. Produced vaccine potency
was evaluated using mice inoculation assay indicating that the ED50 of
test vaccine was >2.5 IU according to the WHO regulation. Immune
response was monitored on both cellular and humoral level revealing that
anti rabies IgG was increasing relative to time and the same to IFN-γ
and IL-5 IFN of local vaccine was significantly elevated than that in
case of H2O2 prepared one.
Introduction
According to the World Health Organization (WHO)
estimates, the number of human rabies deaths in Asia is more than 31,000
per year, of which more than 20,000 occur in India alone. India thus
accounts for 36 % of the global human rabies death burden. Rabies is
endemic in India except in Andaman and Nicobar and Lakshadweep islands,
which are historically known to be rabies-free. The extent of rabies
burden among animals in the country is not exactly known, but the
incidence of the disease is quite high, and the disease is frequently
encountered in different parts of the country. The description of the
outbreaks of rabies in animals during the years 1996 to 2004 reported to
the World Organization for Animal Health (OIE). India reported 586
outbreaks among different species of animals leading to death of 2,463
animals during this period.
During the period 2005 to 2011, 398 outbreaks of
rabies in animals were reported. Many areas of the country did not
report any case during this long period of 7 years despite the endemic
status of rabies there. The actual numbers, therefore, may be
substantially higher, considering the possibility of underreporting due
to weak rabies surveillance and inadequate reporting mechanism in the
country [1]. Rabies is a single strand RNA virus belonging to the
Rhabdoviridae family. Rabies infection is an ancient disease with a high
mortality rate in human and animal population. Based on the World
Health Organization reports, annually between 30000 and 70000 deaths
occurred throughout the world due to rabies infection [2]. Rabies
transmission from animal to animal or to human occurs by
exposure to saliva mainly through animal bites. Other sources of viral
infection may include exposure to scratches, immunization with
incompletely inactivated vaccine, transplantation of virus-infected
organs and virus inhalation.
Rabies is a disease infecting mammal involving dogs,
wolves, foxes, raccoons, cats and bats which serve as reservoirs or
vectors [3]. Rabies virus inactivation is a critical step in production
of vaccines and diagnostic reagents. The recommended inactivating agent
used in rabies vaccine production is beta-propiolactone (βL), but it is a
very expensive chemical and proved to be potential carcinogen. In vitro
studies on nucleic acids extracted from Escherichia coli showed that PL
produces complexes between DNA and proteins [4]. Many studies in
different experimental animals showed that βL caused tumors at various
tissue sites. Thus, it is necessary to find replacement inactivating
agents which are not expensive, safe and available. Hydrogen peroxide (H2O2)
is a strong oxidizing agent. Many studies investigated its ability to
preserve antigenic epitopes and other studies used it as inactivating
agent for development of viral vaccines against both DNA and RNA viruses
including Lymphocytic Choriomeningitis Virus (LCMV), Yellow Fever Virus
(YFV), West Nile Virus (WNV), Vaccinia virus (VV) and Monkeypox Virus
(MPV) [5,6].
Materials and Methods
Rabies virus strain FRV/K1 was supplied from Dr Aly
Fahmy Mohamed; Ex-Head of R&D Sector VACSERA as the aliquot of
infectivity titer of 7.5 log10/ 1ml.
Virus Titration
FRV/K2 virus samples were 10-fold diluted in Hanks Balanced
Salt Solution HBSS (10-1 -10-8). Each dilution was injected
intracraeneally as 0.01-0.03 ml/BALB/cJ mouse. (15/17 gm),
purchased from Research Institute of Ophthalmology. Injected
mice were observed for 15 days for detection of mortality and
mobility. Infectivity titre was calculated according to (Reed and
Muench,1938).
According to the following equation
PD= M>50-50 constant X log dilute / M>50 – M<50
Mice Vaccination
Three groups of mice 10 each were vaccinated using 0.1 mL
of H2O2 inactivated vaccine, the second group was vaccinated
using BPL inactivated rabies vaccine purchased from VACSERA
and third was negative control (not vaccinated). Immune
response regarding cellular and humoral immune response was
considered (total IgG, IFN-γ and IL-5 using ELISA (Bio-Science-
USA).
Virus inactivation
Rabies virus was inactivated using hydrogen peroxide as
0.1 M rabies treated samples were collected at 30 min interval.
Infectivity titre of collected H2O2 inactivated samples was
determined in weaning BALB/cJ mice; (15/17 gm). Inoculated
mice were observed for 15 days and also mortality was recorded.
The infectivity titre was calculated according to (Reed and
Muench, 1938).
Cell culture
Tissue culture flasks were microscopically examined for
confluency. Cells were treated with trypsin EDTA solution 0.25%
(AMRESCO-USA) according to manufacturer protocols. Trypsin
was decanted post cell treatment cells were subjected to the
trace of trypsin solution for 5 min. at 37 °C (Jouan-Franc). Cells
were observed under inverted microscope (Hund-Germany) till
cell dissociated. Growth medium was added to trypsinized cells.
Cells were counted using trypan blue exclusion assay. Cells were
dispensed in new tissue culture flasks according to the time of
need.
Cell count = No. of cells ×Dilution factor × Volume ×104
Vaccine preparation
Exhausted growth media of culture flasks was decanted,
and rabies virus was inoculated as 1 MOI (multiplicity of
infection). Cells were incubated for 1-1/2 hr at 37 °C with 15
hr hour interval shaking for good virus distribution on the cell.
Maintenance medium was added to infected flasks as 75–100ml.
Non-infected cells were included. Cells were observed daily
for detection of cellular changes. Maintenance medium was
collected at 4-5day interval. Harvested medium was clarified
using membrane filtration (Millipore-USA). Each harvest was
titrated as previous in mice to manage the concentration-time by
hollow fibre cartridge (AMICON-USA). Concentrated virus was
titrated as previous.
Vaccine potency
Potency of test vaccine was evaluated using National
Institute of Health (NIH) protocol. Vaccine was fivefold diluted.
Each dilution was inoculated as 0.5 ml/mouse (10/group).
Second dose was administered on the 7th day of prime one on
14th day immunized mice were challenged using challenge virus
standard (CVS) used as 12.5-50 LD50. Mortality was recorded
started from, 5th to 15th days post-infection. Vaccine potency was
calculated according to WHO protocol.
Result
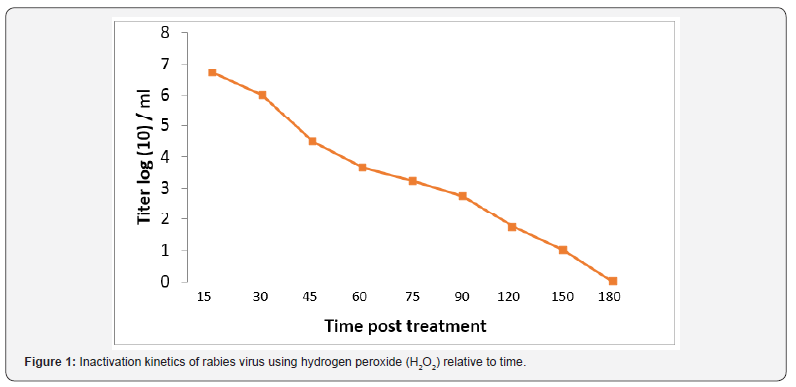
The role of hydrogen peroxide (H2O2) as an inactivant was
traced via evaluation of inactivation kinetics of rabies virus
infectivity, as infectivity titer was decreased relative to time as
H2O2 induced a fast inactivation potential recoding a depletion
rate in the order of 0.03 log (10) /min (Figure 1). In the meantime,
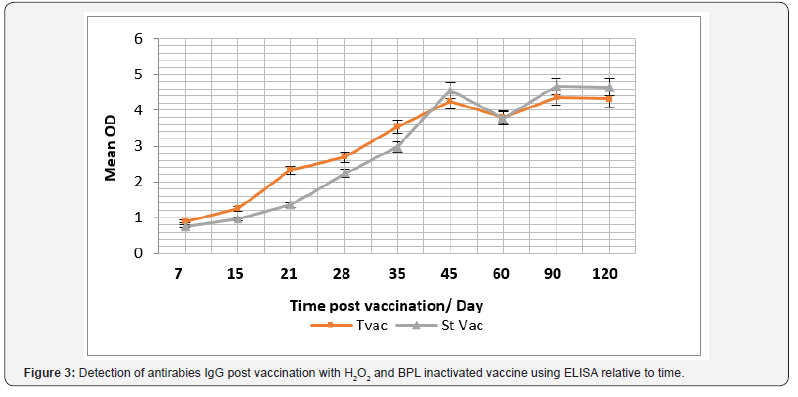
immunogenicity of the produced vaccine was compared with
currently used vaccine purchased from the local market as
immunogenicity was considered concerning total IgG, Interferon
(IFN-γ) and Interleukin – type-5 (IL-5). Data reported revealed
that antirabies total IgG was increased relative to time and there
was an insignificant difference (P>0.05) between antirabies
antibodies elicited post vaccination with H2O2 produced vaccine
and purchased BPL inactivated one, the maximum antirabies
detected on the 45th day post vaccination in both vaccines (P
<0.05) , and post boosting there was a 2dry elevated IgG that
showed an almost stationary phase of antibody recording an
insignificant difference compared with those induced in case
of application of purchased vaccine (P>0.05) and prepared one
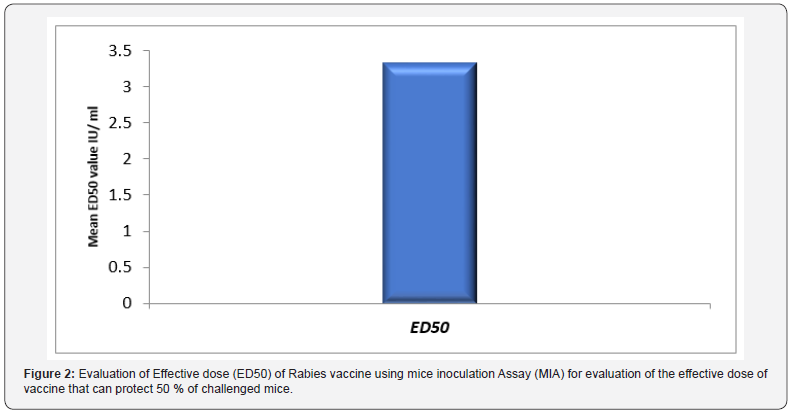
(Figure 2). Vaccine potency was recorded as > 3.5 IU / ml that
was in alignment with the WHO regulation.
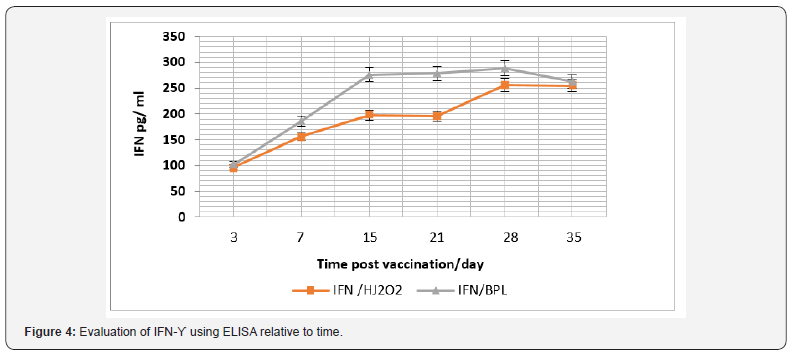
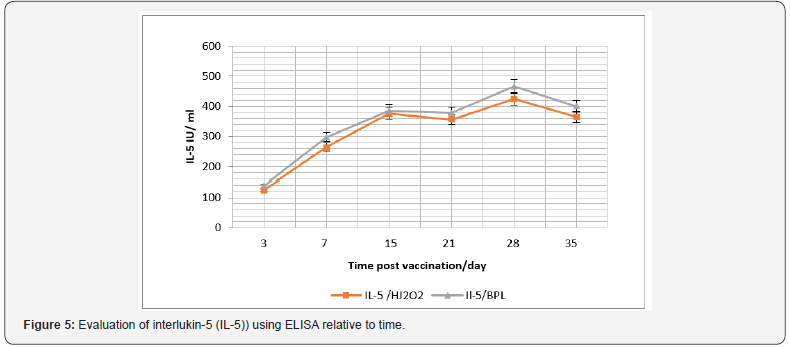
In the same context, cellular immune response was
considered and IFN-γ and IL-5, were monitored (Figure 3). Data
recorded revealed that there was a significant difference in the
IFN-γ level in case of vaccination using purchased vaccine than
that induced post vaccination with H2O2 prepared vaccine during
the 15th and 21th -day post vaccination (P<0.045), and its level
was relative to time post vaccination (Figure 4). While there was
a non-significant difference (P>0.05) in the IL-5 level I case of
vaccination using both vaccine candidates (Figure 5).
Discussion
Rabies virus is an envelope one. It has a single-stranded
and negative-sense RNA genome [7]. Two major structural
components of rhabdoviruses; helical Ribonucleoprotein Core
(RNP) and surrounding envelop. RNP associates with two
proteins which are P, and L proteins. The glycoprotein forms
approximately 400 trimeric spikes, which are tightly arranged on
the surface of the virus [8]. The protein that plays an important
role in replication and transcription in rabies virus is known as
nucleoprotein (N. Both viral transcription and replication are
reduced if the nucleoprotein is not phosphorylated [9]. H2O2 is
a potent oxidizer utilized by neutrophils and other mammalian
cells to inactivate intracellular/phagocytosed pathogens [10,11]
and has been shown in vitro to inactivate a broad range of
microbes [12,13]. Oxidation by H2O2 is believed to inactivate
microbes by several mechanisms, including disruption of lipid
membrane bilayers, oxidation of protein backbones and amino
acid side chains, and oxidation of nucleosides [14,15].
H2O2 has antimicrobial and antiseptic property. It can be
used for sterilization of different surfaces and surgical tools due
to its effectiveness against the wide range of viruses, bacteria
and bacterial spores [16]. βPL, another common inactivation cagent, degrades in solution to undetectable levels within 10-12
h, and in some cases is unable to fully inactivate virus spiked
into vaccine lots at late points in the inactivation process [17].
In-contrast, H2O2 retains its inactivation potential at later time
points during the manufacturing process, providing a robust
approach to virus inactivation and vaccine development, while
maintaining antigenic epitopic pattern the same [18]. H2O2 as
inactivant could be used in preparation of inactivated WNV-KV
retains Env-specific neutralizing epitopes and maintains longterm
stability [18].
On the contratry of our data, H2O2 doesn’t rapidly inactivate
RNA viruses only but also can inactivate DNA viruses with
minimal damage to antigenic structure or immunogenicity. H2O2
has a highly effective method when compared with conventional
vaccine inactivation approaches such as formaldehyde or
β-propiolactone. Mice immunized with H2O2 inactivated
Lymphocytic Choriomeningitis Virus (LCMV) generated
cytolytic, multifunctional virus-specific CD8+ T cells that
conferred protection against chronic LCMV infection [19]. The
H2O2 inactivated West Nile virus- Kunjin strain vaccine is safe
and immunogenic. Also, the H2O2 inactivated West Nile virus-
Kunjin strain may be suitable for protection against WNV (WNVKUNV)
infection in vulnerable populations [20]. In accordance
with our data concerning total IgG level, effective neutralizing
antibody responses could be induced by H2O2 inactivated WNVNY
in BALB/c mice [21]. The protective capacity of a novel
H2O2 WNV-KUNV vaccine against lethal WNV challenge was
demonstrated.
A significant WNV E-protein-specific and neutralizing
antibody response that was enhanced by boosting was observed
by the following vaccination with H2O2 WNV-KUNV in both young
and old mice. H2O2-WNV-KUNV prepared vaccine generates a
poly-functional antigen-specific CD8+ T cell Response [20]. H2O2
WNVKUNV could stimulate induction of protective antibody
and cellular mediator producers (CD8+ T cell response) due
to the purity of the vaccine preparation [20]. H2O2 WNV-KUNV
also induced a robust polyfunctional CD8+ T cell response in
the HLA-A2 human MHC class I transgenic mice, where in the
immunodominant CD8+ T cell epitopes against WNV maps to the
SVG9 peptide in the E protein [22]. Aged mice developed strong
WNV-specific humoral responses and were protected after
immunization and boosting with H2O2 WNV-KUNV was a first
step in demonstrating vaccine efficacy in a highly susceptible
population [20]. βPL, another common inactivation agent,
degrades in solution to undetectable levels within 10–12 hours,
and in some cases is unable to fully inactivate virus spiked into
vaccine lots at late points in the inactivation process [23], by
contrast, H2O2 retains its inactivation potential at later time
points during the manufacturing process, providing a robust
approach to virus inactivation and vaccine development while
still maintaining antigenic epitopes.
In a current case, an independent group compared
γ-irradiation to H2O2 treatment for the development of a vaccine
against Ebola [23]. Interestingly, γ-irradiation resulted in a
damaged vaccine that provided no protection against viremia
and all of the vaccinated Neighborhood Health Plan (NHP) died
or required euthanasia after lethal Ebola challenge. In contrast,
a similar vaccine that was treated with H2O2 provided completed
protection against viremia and the H2O2 Ebola immunized
NHP survived a normally lethal dose of Ebola, suggesting
that key antigenic epitopes were maintained following H2O2
exposure [24]. Vaccine efficacy and its ability to protect against
the disease were detected by using evaluation of the vaccine
immunogenicity test. When H2O2 -inactivated virus suspension
was compared against βPL-inactivated virus suspension for
induction of antibodies in experimental mice, H2O2 -inactivated
virus suspension was proved to be immunogenic and showed
insignificant different response [25]. Results of the NIH potency
testing was in agreement with that requirement of the WHO,
European Pharmacopoeia and U.S. Pharmacopoeia [26-28].
H2O2 -inactivated virus suspension showed accepted potency,
comparable to that of βPL-inactivated virus suspension. Virus
inactivation by H2O2, but not by UV or by short-duration and
higher temperature formalin treatment, is able to maintain the
antigenic structure of the Japanese Encephalitis Virus (JEV) E
protein [29].
In previous study, it confirms that the ability of H2O2 at a
final concentration of 3% to achieve a complete and irreversible
inactivation of fixed rabies virus when incubated for 2 h at
2-8oC, where the virus dropped below limit of detection. It was
noted that the inactivation process using H2O2 was much less
time-consuming than inactivation process using βPL which
requires 24 hrs and that what was on the contrary of our results
[25], that βPL could inactivate rabies virus within 2 hrs. Also,
El-Karamany explained the delay of inactivation is attributed
to the preservation of βPL at -80 as BPL must be kept at -20oC
[30]. One of the important characteristics of a strong inactivating
agent to be used in production of vaccines is that it does not
cause the destruction of antigenic epitopes. This is considered
an essential advantage of H2O2 and it was proved by comparing
H2O2 inactivated virus suspension with the same virus harvest
inactivated using βPL and two commercially available vaccines
using ELISA technique [25].
Formaldehyde is used also as inactivation on poliovirus.
The ability of PV to bind hPVR is reduced due the effect of
inactivation with formaldehyde on early steps of viral replication
[31]. Treatment with formaldehyde had a slight effect on
the immunogenicity in mice of the viral preparations tested.
This effect could be due to the partial destruction of specific
D-antigenic epitopes known to occur during the inactivation
process [32]. Regarding the use of different inactivants and
relate vaccine immunogenicity. It was reported that the effect of
three types of inactivating agent is compared against Infectious
hematopoietic necrosis virus (IHNV). Also, it was explained
the variable antigenicity and immunogenicity of RVFV vaccine
was due to the deterioration of viral epitopes under the effect of Formalin, βPL and BEI as inactivate [33]. The βPL group had
highest level of IgM in both in serum and mucus samples after
vaccination. However, the formaldehyde group had the lowest
level of IgM, which was likely due to antigen modification caused
by the inactivating agent [34]. Formaldehyde is a poly-functional
alkylating agent that modifies carboxyl, hydroxyl, and sulfhydryl
groups of proteins, as well as adenine and guanine [35]. Thus,
it is possible that formaldehyde destroys the immunogenicity
of viral antigens, while βPL and BEI primarily introduce nucleic
acid adducts.
Regarding the immune response, it was reported that all
dogs vaccinated with ETHIORAB rabies vaccine showed a good
immune response to rabies virus and have a rapidly developed a
high titer of rabies virus neutralizing antibodies, demonstrating
that the experimental vaccine was highly immunogenic [36].
The antibody levels peaked at 30-60 days after vaccination with
ETHIORAB and then progressively declined [37]. Antibody titers
rose rapidly as early as day 7 and all dogs had antibody titers
above the WHO-recommended seroconversion threshold (≥ 0.5
IU/ml) [38-40]. Moreover, the absence of any ruffling, partial
paralysis, paralysis and death after intracerebral inoculation
in mice and vaccination in dogs with ETHIORAB rabies vaccine
indicates that the vaccine is safe, free from extraneous agents,
complete inactivation of the virus and efficiently acceptable for
vaccinations against rabies in dogs.
Moreover, using cell culture prepared vaccines are not
only leading to short-term therapy but also causes an efficient
immunity without contraindication or side effects. The efficiency
of Rabisin vaccine is evaluated in field dogs in Tunisia and
reported that at 1-month post-vaccination, the mean rabies virus
neutralizing antibody titers of dogs vaccinated with the Rabisin
vaccine was 4 IU/ml. This study is in line with the present study
and supports the use of the ETHIORAB vaccine in replacement of
the nerve-tissue vaccines [42]. In agreement with our findings,
similar studies reported that showed owned dogs, vaccinated
subcutaneously with a cell-culture-derived vaccine, exhibited
very rapidly decreased neutralizing antibody titers 60 days postvaccination
[43]. Contradictory to this finding a study previously
reported, primary vaccinated with either a Semple type rabies
vaccine or a cell culture-derived vaccine, developed a low level
of neutralizing antibody and 1-month post-vaccination, mean
rabies virus neutralizing antibody titers were 0.37 and 0.46
IU/ml, respectively. However, a booster injection after 1 year,
showed that dogs immunized with cell-culture vaccine had
a higher a virus neutralizing antibody titer than the animals
vaccinated with the nerve-tissue vaccine (1.27 IU/ml versus
0.44 IU/ml) [44-50].
Conclusion
From the introduced data it can be concluded that H2O2 as
inactivating agent showed an equivalent efficacy as inactivant
like in case of use of βPL. Also, Prepared Rabies vaccine was
immunogenic equally to the currently βPL distributed vaccine.
Effect of prepared vaccine immunogenicity b and immune
reactivity is time dependent Finally H2O2 prepared vaccine is
equal potentially to BPL papered vaccine in addition to its safety
measure.
Recommendations
It is recommended to evaluate H2O2 prepared vaccine
stability and side effect to monitor the free Oxygen effect on
recipient animal model. Inactivation of rabies virus at different
thermal conditions using H2O2 as a low cost and non-oncogenic
inactivate.
To know more about Open Access International
Journal of Pulmonary & Respiratory Sciences please click on: https://juniperpublishers.com/ijoprs/index.php
To know more about Open access Journals
Publishers please click on : Juniper Publishers
To know more about juniper publishers: https://juniperpublishers.business.site/


Comments
Post a Comment